freedomchurch
数十年的研究确定了免疫系统复杂结构在整个生命周期的健康过程中的重要性,而两种标记物细胞因子白介素6(IL-6)和急性期蛋白C反应蛋白(CRP)对免疫系统至关重要。
谈到IL-6和CRP最先想到的应该是炎症。但是,最近有研究强调IL-6和CRP不仅与炎症有关,对于整个生命周期的健康也至关重要,这两种生物标记物视为对疾病特异性和全因死亡率至关重要。
在过去的十年中,人格特质与IL-6和CRP都相关的想法越来越受到人们的关注。此前很多研究证据表明,尽职性人格可能有炎症相关的生物标志物的保护作用。近期,爱尔兰利默里克大学领导的开创性研究首次揭示了免疫系统将责任心与长期死亡风险联系在一起,研究结果发表在journal Brain, Behavior, and Immunity上。
Personality pathways to mortality: Interleukin-6 links conscientiousness to mortality risk. DOI: 10.1016/j.bbi.2021.01.032
该研究收集了美国中年纵向研究的数据,对957名成年人进行了为期14年的随访,发现在尽责这一人格特质上得分较低的人,与得分较高的人相比,未来死亡的风险会增加40%。
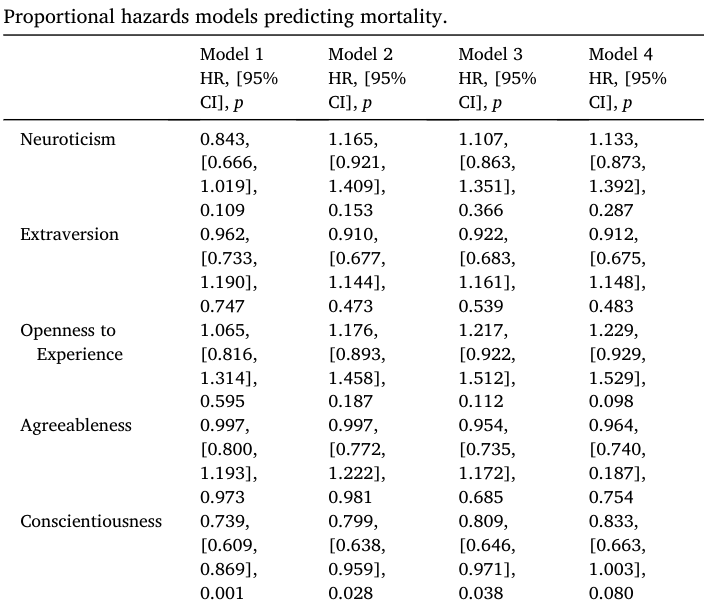
几个基线变量对死亡率有直接影响
结果显示,自觉性与较低的死亡风险相关(HR = 0.74;p = 0.001;95% CI,0.61-0.87),这样自觉性每增加1 与死亡风险降低35%相关。在引入人口统计学对照(HR = 0.80;p = 0.028;95% CI,0.64-0.96)和健康相关因素(HR = 0.81;p = 0.038;95% CI,0.65-0.97)后,这一效应被减弱。完全调整的基线模型中,IL-6与更大的死亡风险相关(HR = 2.99;p = 0.010;95% CI,0.49 - 5.49)。CRP没有显著关联(HR = 0.91;p = 0.733;95% CI,0.42 - 1.40)
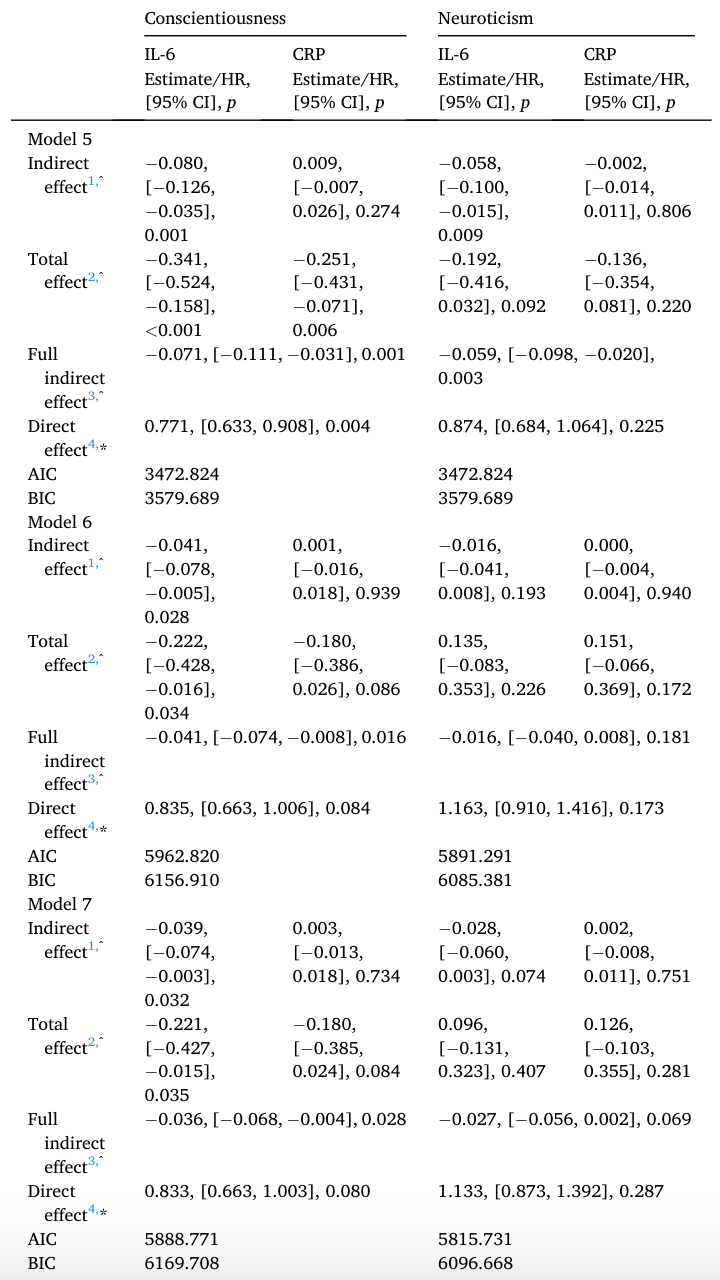
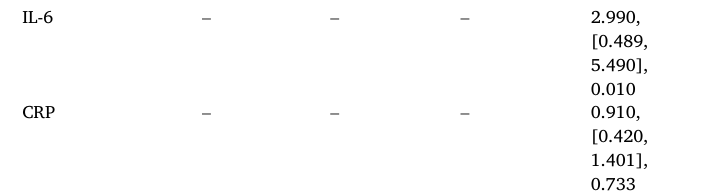
尽职性和神经质性人格的调解模型预测死亡率。
进一步研究显示,IL-6作为尽责性与死亡率之间关系的一个强有力的中介因子出现,尽责性通过IL-6对死亡率的影响的23.46%、18.47%和17.65%。结果表示,尽职认真人格的测试者更长寿且白IL-6的生物标记物水平较低。
研究作者,利默里克大学心理学系和健康研究所Ó Súilleabháin博士表示,众所周知,人格与长期死亡风险有关,但是其中如何运作机制尚未清楚,该研究的结果首次确定了一个潜在的生物标志物直接将个性与长期死亡风险联系起来。通过复制,这些发现为未来的干预措施提供了一个机会,以增加我们的寿命和整个生命周期的健康。
该研究具有理论和实践意义。人格与健康的理论模型通常侧重于行为机制; 这项研究确定并提供了生物学途径的证据。关于人格和死亡率的研究表明,心理因素可能有助于确定谁最有可能过早死亡以及为什么。在未来的工作中,测试个性化信息干预措施对改善健康结果,包括降低过早死亡风险的有用性将至关重要。
值得提出的是,尽管该研究具有多种优势,例如广泛的随访期和代表已知全因死亡率的预测因素的多种数据形式。但还应注意局限性。尽管这项研究专门针对IL-6和CRP,但仍需要进一步研究以检查其他可能相关的促炎和抗炎细胞因子,重要的是,目前的发现可能如何与其他细胞因子相互作用,激素和其他生物标记物作为介导途径可能很复杂。
总之,该结果表明,尽职尽责的人寿命更长,部分原因是其IL-6的循环水平较低。这些结果为将这种人格特质与长寿联系起来的生物学机制提供了重要的见识。在此过程中,强调了重要性,并需要确定生物学途径,以弥合这种从人格到未来工作的未来死亡风险的联系。这项研究为人格健康难题提供了至关重要的部分,表明炎症和衰老过程的核心生物标志物IL-6提供了一条途径,部分解释了尽职调查与长期死亡风险相关的原因。
原始出处:
Páraic S. O'Súilleabháin, Nicholas A. Turiano, Denis Gerstorf, Martina Luchetti, Stephen Gallagher, Amanda A. Sesker, Antonio Terracciano, Angelina R. Sutin. Personality pathways to mortality: Interleukin-6 links conscientiousness to mortality risk. Brain, Behavior, and Immunity, 2021; DOI: 10.1016/j.bbi.2021.01.032
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#HAV#
40
#EHA#
0
已学习已分享
76
谢谢分享
67
好文章!
71
有意思
72