急性冠状动脉综合征( ACS)主要是指冠状动脉粥样硬化斑块破裂或侵蚀,继发完全或不完全闭塞性血栓形成,所引起的急性心肌缺血综合征,包括 ST 段抬高型心肌梗死(STEMI)、 非ST段抬高型心肌梗死(NSTEMI)和不稳定性心绞痛(UA)。
ACS的症状复杂多样,主要表现为发作性胸痛、胸闷等,有些患者病情发作急骤,病情迅速恶化,短时间内危及患者的生命。因此,早期发现ACS患者、找出病因、全程规范管理,对挽救患者生命,改善生存质量有着重要的意义。
那么,临床上遇见ACS的患者,诊断思路是什么?处理原则是什么?本文整理了 ACS的相关内容,供大家学习参考。
一、如何快速诊断ACS?
ACS的发病率在我国依然呈逐年增加的态势,且绝大多数ACS患者首诊于急诊科。胸痛患者首诊于急诊科,皆应快速询问病史、体格检查、评估生命体征,并尽可能短的时间内完成标准心电图、心肌损伤标记物检查,作出初始诊断。值得注意的是,胸痛或胸闷不适是ACS患者最常见的临床表现,但部分患者尤其老年、女性和糖尿病等患者的症状可不典型,应提高警惕。
1,病史询问
1)现病史:发病时间、症状及治疗情况。重点询问有无胸痛、胸闷、剑突下不适、呼吸困难等症状,以及症状持续或缓解的时间,是否有其他伴随症状。是否有冠心病相关不良个人生活习惯,如吸烟、酗酒、生活节律混乱、缺乏运动、精神压力过大等。
2)既往史:有无心血管危险因素,比如高血压、糖尿病、高胆固醇血症、肥胖/超重等、心脏基础疾病等。同时,要询问并记录各类出血性疾病史。
3)家族史:是否有早发冠心病、卒中等家族史。同时,要询问是否存在工作或家庭人际关系不和谐等。
2,体格检查
对患者进行全面查体,重点检查生命体征,包括血压、心率、呼吸频率,血氧饱和度、心律等。此外,还需要必要的辅助检查包括12/18 导联心电图检查、血常规、超敏肌钙蛋白、冠状动脉造影、超声心动图、运动心电图、放射性核素检查、冠状动脉 CT 血管造影(CTA)、肾功能等。
3,心电图
心电图对 ACS的诊断有一定的价值。当原有左束支阻滞患者发生心肌梗死时,心电图诊断困难,需结合临床情况仔细判断。单次心电图对NSTEMI诊断价值有限,宜连续、动态记录。
4,肌钙蛋白
肌钙蛋白是一种蛋白质络合物,是横纹肌收缩的一种调节蛋白,是骨骼肌和心肌的结构蛋白。心肌肌钙蛋白T和肌钙蛋白I具有心肌特异性,用于ACS的实验室诊断。如不能检测心肌肌钙蛋白T,可用肌酸激酶同工酶-MB (CK-MB)检测作为替代。
5,超声心动图
超声心动图评估心脏结构、运动与功能,同时具有确诊或鉴别诊断意义。如果患者无反复胸痛、心电图结果正常、心肌肌钙蛋白T/肌钙蛋白I水平正常,但仍疑似ACS,建议行无创负荷试验以诱发缺血发作,视结果再进一步考虑是否行有创检查。另外,如果心肌肌钙蛋白T/肌钙蛋白I和 (或)心电图结果正常,但仍疑似ACS,建议行多排螺旋计算机断层扫描(MDCT)冠脉造影检查。
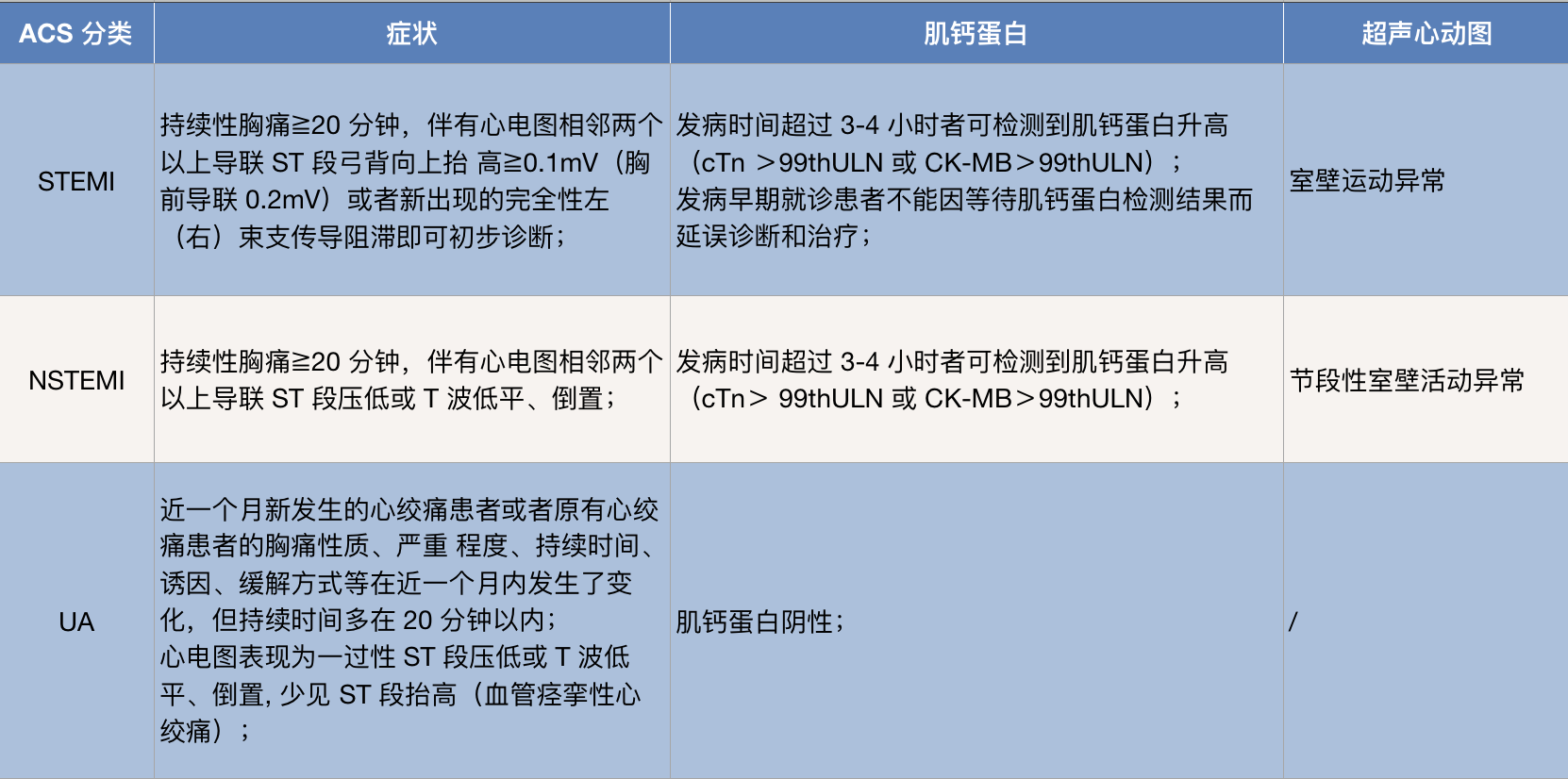
ACS的诊断标准
二、ACS患者如何风险评估?
ACS患者的风险评估是一个连续的过程,需要根据患者的临床情况进行动态考量。
1,STEMI患者
高龄、女性、Killip II~IV级、既往心肌梗死史、心房颤动、肺部啰音、收 缩 压< 100mmHg、心率 >100次/min、糖尿病、肌酐增高、BNP或 NT-proBNP明显升高等均是STEMI患者死亡风险增加的独立危险因素。溶栓治疗失败、伴有右心室梗死和血流动力学 异常的下 壁STEMI患者病死率增高。合并机械性并发症的STEMI患者死亡风险增大。冠状动脉造影可为STEMI危险分层提供重要信息。
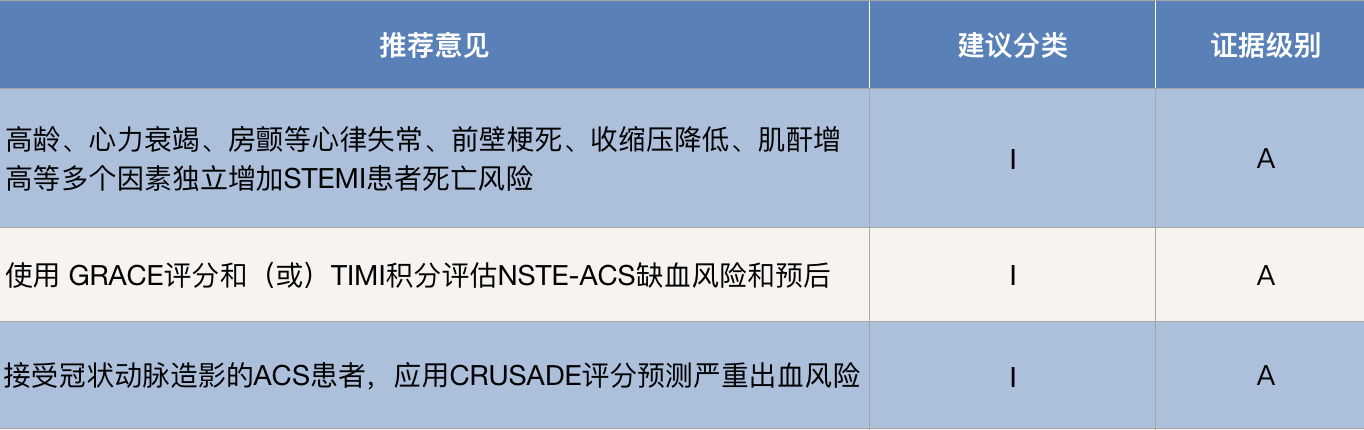
ACS的风险评估
2,NSTE-ACS 患者
NSTE-ACS 患者可使用确定的风险评分体系进行病情和预后评估。①缺血风险:GRACE评分对NSTE-ACS患者提供了较为准确的风险 评估。在GRACE评分基础上,GRACE2.0风险计算可直接评估住院、6个月、1年 和3年的病死率,同时还能提供1年死亡或心肌梗 死的联合风险。②出血风险:对于接受冠状动脉造影的ACS患者,CRUSADE评分对严重出血具有合理的预测价值。
三、如何有效治疗ACS?
1,ACS的处理原则
首先要快速排除最危险、最紧急的疾病。对危及生命的ACS一旦确诊,即应纳入快速通道。同时,在最短的时间内解除或缓解心肌缺血,严防恶性事件的发生,降低医疗费用。所有医院和医疗救急系统必须记录和监测时间延误,努力达到并坚守下列质量标准:
★首次医疗接触到记录首份心电图的时间小于10分钟。
★首次医疗接触到实施再灌注的时间,溶栓小于30分钟,直接PCI小于90分钟,如果症状发作在120分钟之内或直接到能够实施PCI的医院,则小于60分钟。
2,STEMI患者的治疗
对于 STEMI 患者应尽早、快速和完全地开通梗死相关动脉,同时进行规范的药物治疗。
就诊于有急诊介入治疗能力医院的患者,首选直接经皮冠状动脉介入治疗(PPCI)策略。同时,在药物治疗中,双联抗血小板,优先选择阿司匹林联合替格瑞洛,或阿司匹林联合氯吡格雷、抗凝、调脂、抗心肌缺血、 抗心衰、抗休克的规范化药物治疗方案。
对于就诊于无急诊介入治疗能力医院的患者,综合评估转运时间、症状发生时间、并发症风险、药物溶栓出血风险,选择转运 PPCI 策略或溶栓后转运策略。
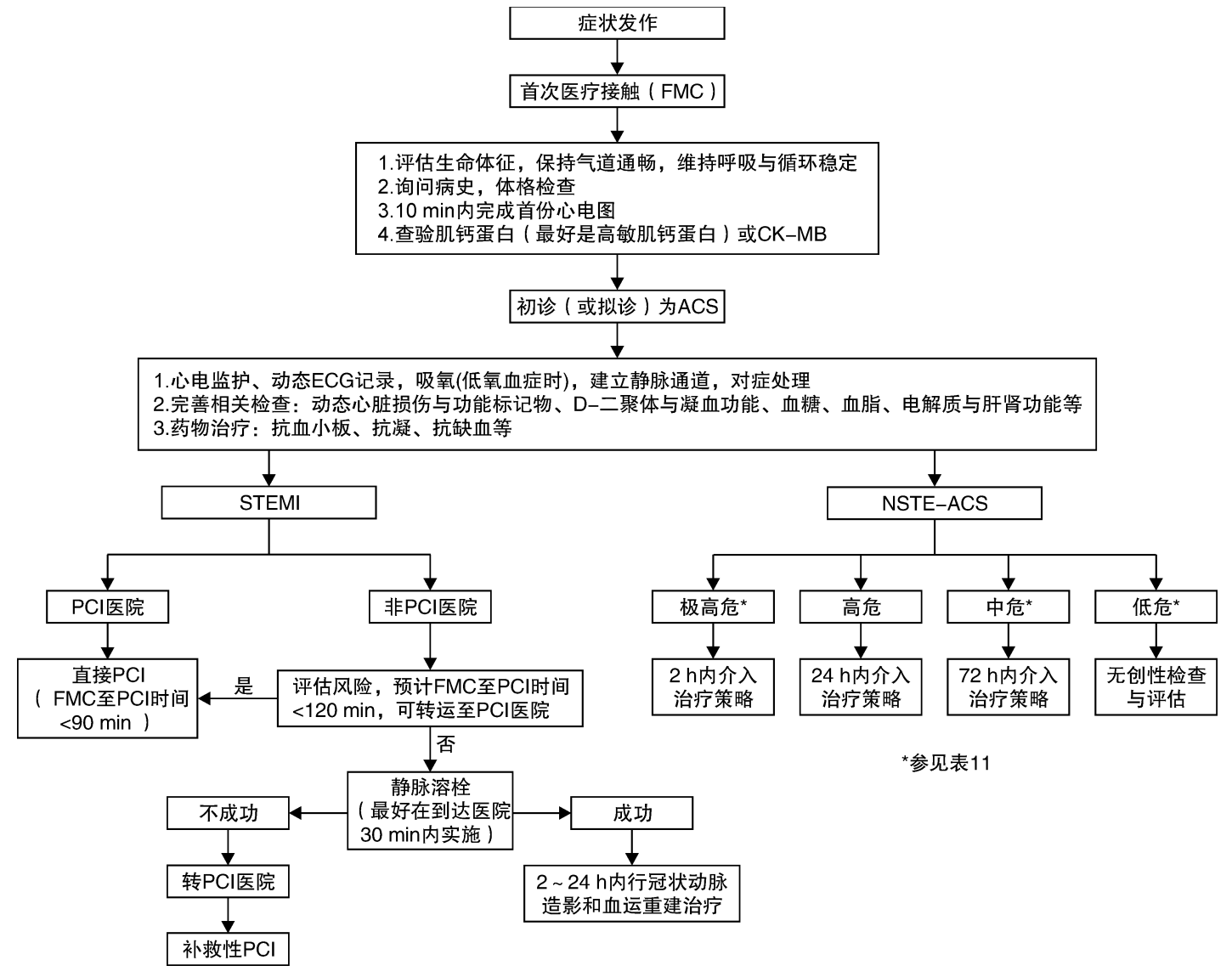
ACS 患者诊疗流程
3,NSTE-ACS 患者的治疗
1)一般治疗:
NSTE-ACS 患者的一般治疗包括镇静镇痛、稳定生命体征,辅助氧疗。对没有禁忌症且给予最大耐受剂量抗心肌缺血药之后仍然有持续缺血性胸痛的 NSTE-ACS 患者,可静脉注射吗啡。经过规范药物治疗生命体征难以稳定的患者应及时给予循环或/和呼吸支持。
2)药物治疗:
双联抗血小板、抗凝、调脂、抗心肌缺 血、抗心衰、抗休克的规范化药物治疗方案。其中,双联抗血小板优先选择阿司匹林联合替格瑞洛,或阿司匹林联合氯吡格雷。
3)介入治疗:
对于就诊于有急诊介入治疗能力医院的极高危或高危患者,应分别在 2 小时内或 24 小时内实施紧急或早期介入治疗;
对于中危患者,可以在进行充分药物治疗基础上,在 72 小时内实施延迟介入治疗;
对于低危患者,在药物治疗基础 上根据无创检查结果决定是否需要接受介入治疗;
四、ACS 患者的随访管理
根据ACS患者病情制定出院计划和随访方案,在出院前进行风险评估,分为低危患者和中、高危患者。对于中、高危患者出院后 1 年内进行随访,至少 1-3 个月1次, 其中出院后 1、3、6、12 个月必须随访。另外,根据患者症状、体征和辅助检查结果,评估并监控 ACS 患者病情,及时调整治疗策略。
辅助检查:ACS 患者需要进行超声心动图、24小时动态心电图(特别是心肌梗死伴严重心衰或/和心律失常患者),脑钠肽、血脂水平、 空腹血糖、糖化血红蛋白、血电解质、血常规和凝血常规、肝功能和肾功能等检查。
STEMI患者每3-6个月应检查超声心动图, NSTE-ACS患者可每年检查一次超声心动图。行PPCI患者术后 9-12个月稳定期患者可考虑行运动负荷试验评估心肌缺血情况 和/或行冠状动脉影像学检查评估冠状动脉通畅情况。
用药方案:优化用药方案,提高药物治疗达标率。
1)双联抗血小板治疗:无禁忌证的ACS患者,双联抗血小板治疗至少1年,优 选阿司匹林联合新型P2Y12受体拮抗剂。
2)调脂治疗:所有ACS 患者无论初始低密度脂蛋白胆固醇(LDL-C)水平都应使用最大 可耐受剂量他汀类药物。以LDL-C水平作为干预目标,达标后不 应停药或盲目减少剂量,对于不达标的患者,加用PCSK9抑制 剂或胆固醇吸收抑制剂。
3)β受体阻滞剂治疗:无禁忌证的ACS 患者(所有STEMI和存在持续缺血症状或左室射血分数降低的 NSTE-ACS患者),建议使用β受体阻滞剂,以静息心率为参照, 逐步调整至目标剂量和最大可耐受剂量。
4)ACEI/ARB类药物治 疗:ACEI/ARB类药物用于无禁忌症的STEMI患者和左室射血分 数降低的NSTE-ACS患者,逐步调整至目标剂量和最大可耐受剂 量。建议左室射血分数降低的ACS患者使用ACEI/ARB/ARNI。
5)SGLT2抑制剂(或GLP-1受体激动剂)治疗:合并糖尿病患者若无禁忌,建议使用SGLT2抑制剂(或GLP-1受体激动剂),评估患者治疗依从性。
总之,ACS的治疗需要争分夺秒,根据患者的症状特点,制定合理的诊疗流程,及时明确ACS 的诊断,是有效治疗的开端。
参考资料
1.中华人民共和国国家卫生健康委员会.急性冠状动脉综合征分级诊疗服务技术方案.2021.
2.中国医师协会急诊医师分会,等.急性冠脉综合征急诊快速诊治指南(2019).临床急诊杂志,2019,20(4):253-262.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#冠状动脉综合征#
50
学习了
58
学习,重点记忆
61
学习后收获很大!
61
#综合征#
46
签到
80
学习了
0