Radiology:深度学习在冠状动脉CTA钙化评分的应用
2022-01-15 shaosai MedSci原创
冠状动脉钙化评分(CAC)是一种有效的冠状动脉疾病风险分层的影像学指标。在临床上存在多种类型的钙化评分,其中Agatston钙化评分是使用最为广泛的一项。
 冠状动脉钙化评分(CAC)是一种有效的冠状动脉疾病风险分层的影像学指标。在临床上存在多种类型的钙化评分,其中Agatston钙化评分是使用最为广泛的一项。冠状动脉内的体素如果衰减超过预定的阈值130H以上,就被定义为钙化。然后通过一个预定义的方程式来计算得分。过去采用的是半自动的方法进行计算,近几年,人们尝试在平扫CT中自动计算Agatston评分,其中就包括基于深度学习的计算方法。
冠状动脉钙化评分(CAC)是一种有效的冠状动脉疾病风险分层的影像学指标。在临床上存在多种类型的钙化评分,其中Agatston钙化评分是使用最为广泛的一项。冠状动脉内的体素如果衰减超过预定的阈值130H以上,就被定义为钙化。然后通过一个预定义的方程式来计算得分。过去采用的是半自动的方法进行计算,近几年,人们尝试在平扫CT中自动计算Agatston评分,其中就包括基于深度学习的计算方法。
光谱CT利用了X射线光子衰减的能量依赖性,根据多能级下的材料分解提供更详细的组织分析。通过使用材料分解的虚拟碘减法算法,光谱CT扫描仪能够生成虚拟非强化(VNC)CT扫描。同时,在不需要额外辐射的情况下,成像后的重建可以取代真正的平扫CT。
近日,发表在Radiology杂志的一项研究提出了一种深度学习方法来自动量化CTA的钙化评分,为快速准确的获得钙化评分提供了技术支持。
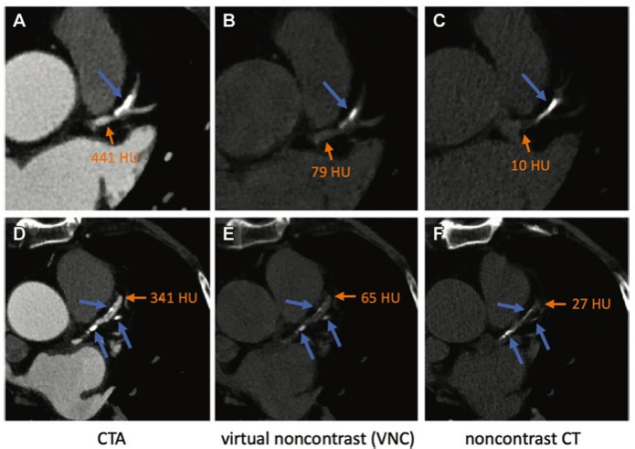
图 (A-F)钙化(蓝色箭头)在两位患者CT血管造影(CTA)、VNC CT和平扫CT扫描中的显示。VNC CT扫描(B,E)和平扫CT扫描(C,F)上的钙化外观相似,使用预定义的阈值130HU可以很容易获得,因为冠状动脉的衰减(B,C,E和F中的橙色箭头)明显小于130HU。然而,通过CTA(A,D)获得冠状动脉钙化(CAC)区域并估计相应的CAC评分可能具有挑战性,因为造影剂增强的动脉衰减不一。
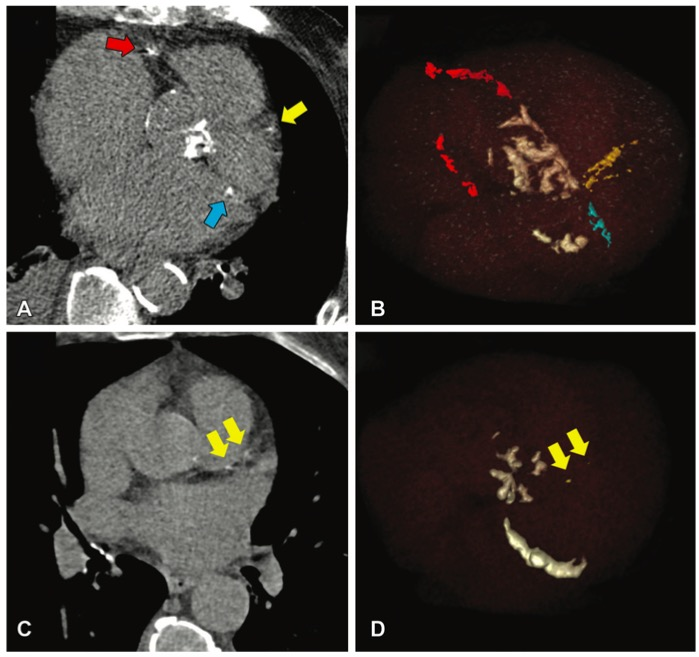
总之,本研究提出了一种深度学习方法来自动量化来自CT血管造影(CTA)图像的冠状动脉钙(CAC)评分。本研究结果表明,所提出的方法可以准确地量化CAC,并对CTA的风险进行分类。
原文出处:
Dan Mu,Junjie Bai,Wenping Chen,et al.Calcium Scoring at Coronary CT Angiography Using Deep Learning.DOI:10.1148/radiol.2021211483
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#CTA#
35
#冠状动脉CT#
30
不错哦
0
钙化积分,cta更加准确
41
学习了
45
学习
54