Liver Cancer:Lenvatinib(仑伐替尼)初始治疗出现应答是仑伐替尼(LEN)+经动脉化疗栓塞(LEN-TACE)序贯治疗的预后指标
2022-02-20 yd2015 MedSci原创
研究表明,对初始LEN治疗有反应的u-HCC患者,LEN-TACE序贯治疗可能比LEN单药治疗提供更多的临床益处。Lenvatinib(仑伐替尼)初始治疗出现应答是LEN-TACE序贯治疗预后因素。
对于不可切除的肝细胞癌(u-HCC), lenvatinib(仑伐替尼)+经动脉化疗栓塞(LEN-TACE)序贯治疗的益处资料有限。因此,近期Liver Cancer杂志上发表了一项研究成果,主要是比较LEN- TRAE序贯治疗与LEN单药治疗不可切除的肝细胞癌(u-HCC)患者的疗效和安全性,并探索了影响LEN-TRAE序贯治疗深度应答的因素。
研究是多中心的队列研究,纳入2018年至2020年期间247例接受LEN治疗的u-HCC患者。倾向评分匹配(PSM)确定了63对具有良好平衡特征的匹配患者。我们回顾性比较了LEN-TACE和LEN单药治疗组的临床结果,包括总生存期(OS)、无进展生存期(PFS)和不良事件发生率(AEs)。此外,我们评估了肿瘤反应、白蛋白-胆红素(ALBI)评分的变化、影响PFS和OS的因素,以及有助于LEN- TRAE序贯治疗深度应答的独立预测因素。在本研究中,首次TACE术后恢复LEN 8周后,“深度应答”定义为mRECIST上达到CR或PR,靶病灶直径和至少减少30%。
在研究期间,247例u-HCC患者接受了LEN治疗。17例患者被排除,因为在给药8周后的初始反应无法评估。其余230例纳入研究的患者被分为LEN- TACE组(n= 63,27.4%)和LEN单药治疗组(n= 167,72.6%)。相对于LEN单药组,LEN- TACE组有MTA治疗史的患者比例显著减少(P=0.002)。此外,在LEN-TACE组中,第8周治疗基于RECIST 1.1和mRECIST标准获得PR的比例均较高(RECIST 1.1: P=0.004, mRECIST: P=0.008)。所有患者的中位随访时间为15.7个月。LEN-TACE组的中位OS为31.2(26.4-34.3)个月,LEN单药治疗组的中位OS为15.7(13.1-19.4)个月, LEN-TACE组的OS显著高于LEN单药治疗组(P=0.001)。此外,LEN-TACE组的中位PFS为12.2(8.5-17.3)个月,明显长于LEN单药治疗组的6.7(5.3-10.2)个月(P=0.025)。
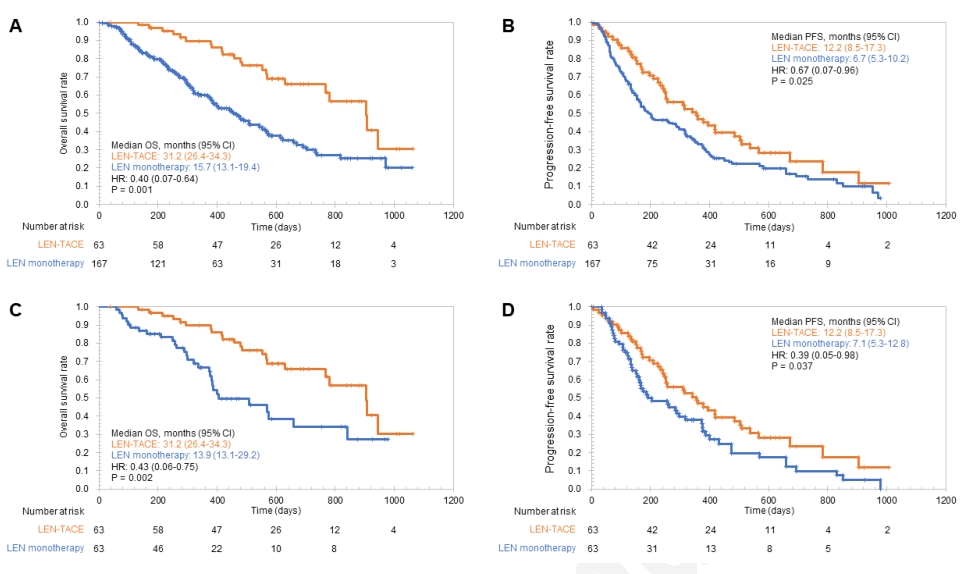
所有患者和PSM队列患者的OS和PFS
PSM队列的中位随访时间为15.6个月。LEN-TACE组的中位OS为31.2(26.4-34.3)个月,LEN单药治疗组的中位OS为13.9(13.1- 29.2)个月。LEN-TACE组OS显著高于LEN单药组(P=0.002)。此外,LEN-TACE组的中位PFS为12.2(8.5-17.3)个月,明显长于LEN单药治疗组的7.1(5.3-12.8)个月(P=0.037)。
根据mRECIST标准,LEN-TACE组TACE治疗8周后CR、PR、SD、PD的患者比例分别为20.6%、41.3%、12.7%、25.4%。ORR和DCR分别为61.9%和74.6%。在BCLC-B期(n=22)的亚组分析中,CR、PR、SD和PD患者的比例分别为14.8%、59.3%、14.8%和11.1%。ORR和DCR分别为74.1%和88.9%。

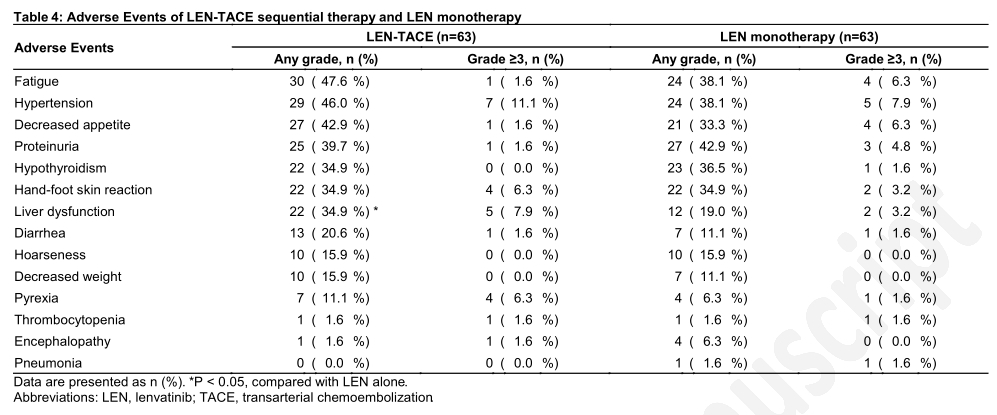
LEN-TACE组中任何级别最常见的AEs为疲劳(47.6%)、高血压(46.0%)和食欲下降(42.9%)。最常见的≧3级AE为高血压(11.1%)。因此,LEN-TACE组具有可接受的安全特性,没有意外的安全信号。LEN单药治疗组最常见的AEs为蛋白尿(42.9%)、手足皮肤反应(34.9%)、疲劳(38.1%)和高血压(38.1%)。最常见的≧3级AE为高血压(7.9%)。
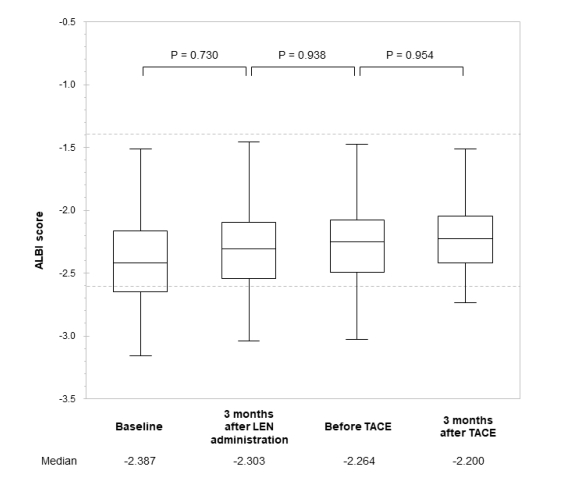
LEN-TACE组患者中,LEN在给药前、给药后3个月、TACE前、TACE后2个月中位ALBI评分分别为-2.38、-2.30、-2.26、-2.20,差异无统计学意义。
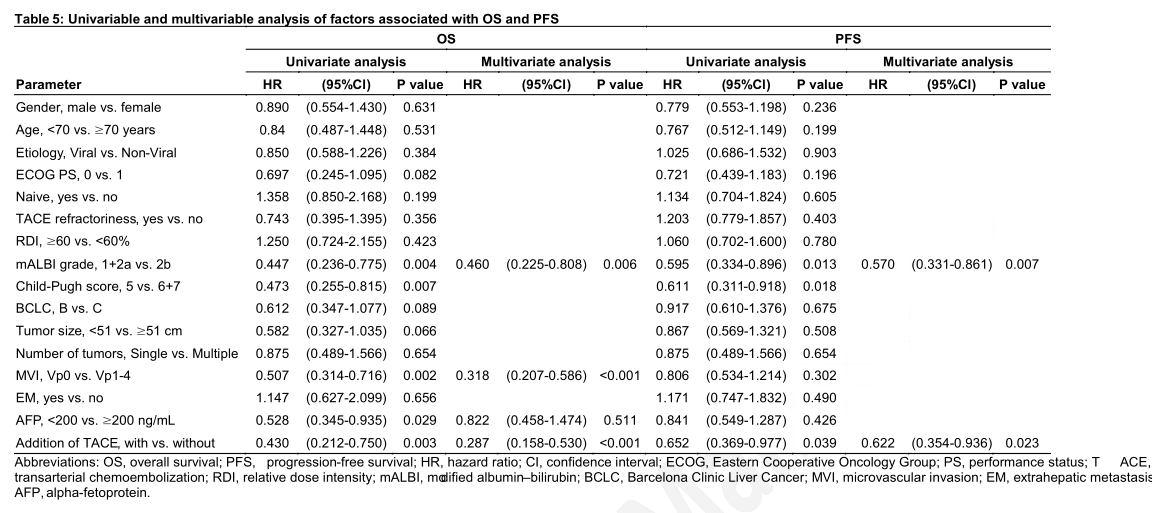
多变量分析显示OS与mALBI 1+2a级(P=0.006)、MVI-Vp0 (P<0.001)和TACE的加入(P<0.001)独立相关;而RFS与mALBI 1+2a级(P=0.007)和TACE的加入 (P=0.023)独立相关。
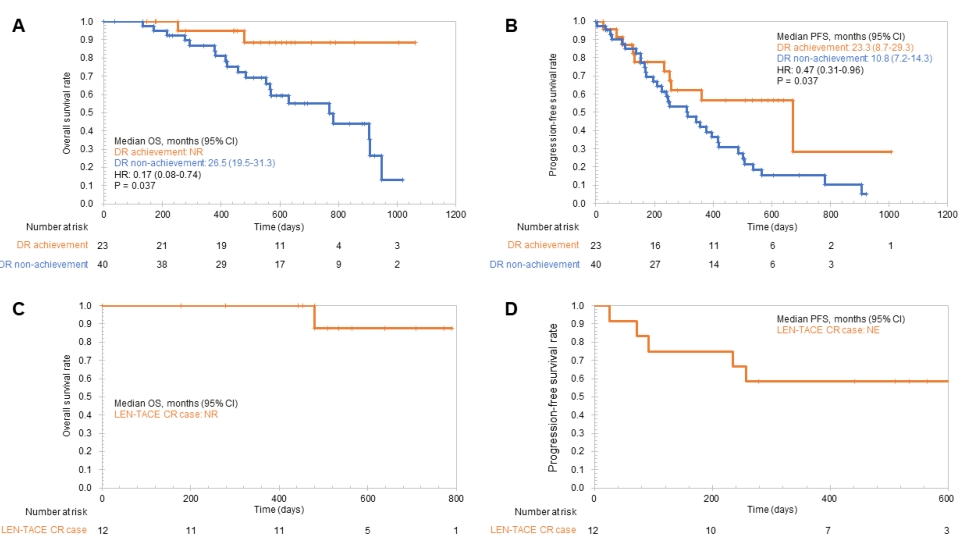
在LEN-TACE组中,23例(36.5%)患者获得深度应答。获得深度应答患者的中位OS未达到,未获得患者的中位OS为26.5个月(19.5-31.3个月),统计学有显著差异(P=0.037)。此外,获得深度应答患者的中位PFS为23.3(8.7-29.3)个月,未获得患者的中位PFS为10.8(7.2-14.3)个月(P=0.037)。
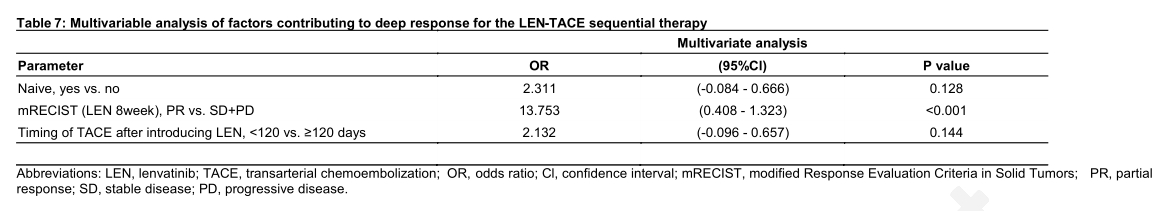
多变量分析显示,深度应答与基于mRECIST标准评估的对LEN的初始肿瘤应答结果独立相关:PR(比值比:13.753,95% CI: 0.408-1.323, P<0.001)。
在本研究中,共有12例患者(19.0%)通过LEN-TACE序贯治疗达到CR,其中2例患者接受了转化手术。CR患者的中位随访时间为17.4个月。CR患者预后良好,1年总生存率(OSR)为100%,2年OSR为87.5%)。5例发现新病灶;3个月无进展生存率为83.3%,6个月为75.0%,12个月为58.3%。
综上,研究表明,对初始LEN治疗有反应的u-HCC患者,LEN-TACE序贯治疗可能比LEN单药治疗提供更多的临床益处。mRECIST评估的对初始LEN治疗出现客观应答是影响LEN-TACE序贯治疗深度应答的独立因素。
原始出处:
Kuroda H, Oikawa T, Ninomiya M, et al. Objective response by mRECIST to initial lenvatinib therapy is an independent factor contributing to deep response in hepatocellular carcinoma treated with lenvatinib-transcatheter arterial chemoembolization sequential therapy. Liver Cancer , DOI: 10.1159/000522424. Published online: February 15, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#初始治疗#
44
#ACE#
32
#TAC#
44
#预后指标#
42
#lenvatinib#
36
#化疗栓塞#
36
此,建立一个基于患者表型或基因交
55