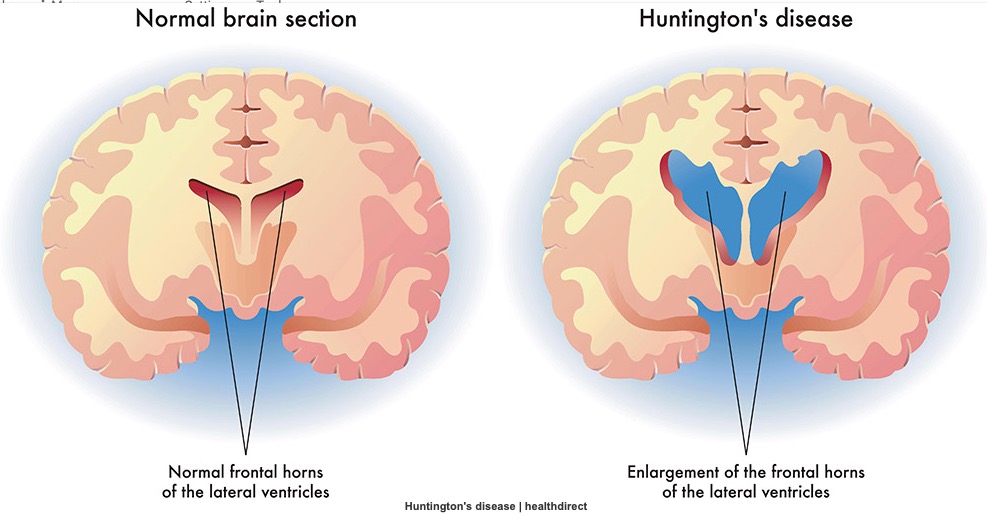
亨廷顿病(HD)是一种中枢神经退行性疾病。主要因大脑中的神经元丧失导致进行性运动异常、认知能力下降并最终死亡。运动障碍通常包括舞蹈症,但也可能涉及肌张力障碍、共济失调、眼运动问题和帕金森病,其中一些最初只能通过有针对性的HD检查来识别。
Healthdirect
不久前,来自英国卡迪夫大学的Branduff McAllister等人发表在《神经病学》(Neurology)杂志上的研究则发现,随着发病年龄的增加,HD的最初表现越来越可能是运动性症状,而较少是精神性症状,且与致病性CAG重复长度无关。
随着神经退行性变的潜在疾病缓解治疗进入第三阶段临床试验,在对症状前HD基因携带者进行治疗之前,识别最早的病理变化至关重要。磁共振成像研究表明,脑萎缩发生在症状出现前15年,然而T1加权结构磁共振成像检测到的信号变化的具体病理来源很难确定。
尸检研究和HD小鼠模型都表明细胞死亡、髓鞘脱失和铁积累在HD发病机制中十分重要,但这些过程之间发生的确切时间和相互作用,以及它们对症状学的影响尚不清楚。
为此,来自英国伦敦大学学院神经病学研究所的专家猜测,HD的病理过程在症状出现前许多年就开始了,并开展了HD的横断面研究,结果发表在《柳叶刀》子刊Ebiomedicine杂志上。
研究人员使用新的成像技术来确定是否可以在同一个群体中检测到整个大脑的宏观和微观结构变化。共纳入62名早发型HD(PreHD)和61名健康对照者。检查了所有参与者灰质和白质体积、通过扩散加权成像(DWI)测量检测白质微结构、根据磁化传递估计髓磷脂和铁含量的多参数图(MPM)、质子密度(PD)等。
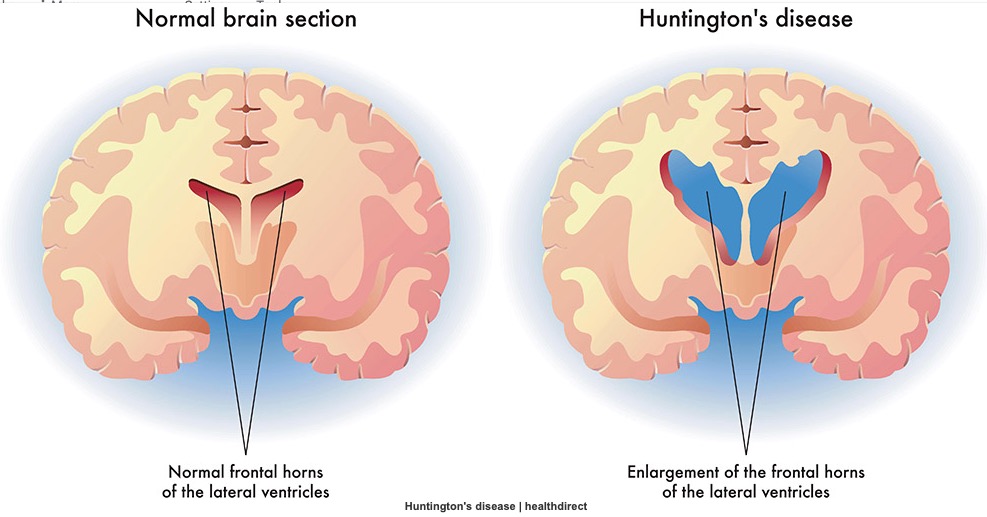
两组MPM和脑脊液中 NfL之间的关系
除了评估PreHD和对照组之间的组差异;还进行了所有影像学指标与疾病负担和脑脊液神经丝光(NfL)之间的相关性研究。
结果显示,与对照组相比,PreHD参与者的壳核、苍白球和外包膜中,R1和R2*显著增加,提示铁沉积增加。低皮质R2*与额叶和顶枕皮质较高的脑脊液NfL之间也有显著关联,提示髓鞘或铁减少。但在校正后的水平上没有其他显著结果。
在MPM的数据中,组间比较的显著结果。a)与对照相比,PreHD苍白球和脑白质壳核的R1值显著增加;b) 与对照相比,PreHD白质外膜中的R2*显著增加。
研究人员指出,皮质下结构和周围白质中铁沉积增加是非常早期的PreHD的特征。此外,脑脊液NfL的增加与后顶叶-枕叶皮层的显微结构变化有关,而后者在既往研究中被证明是HD最早出现的皮层变化。
综上,该研究表明,皮层下和皮层脑区的铁和髓鞘变化在亨廷顿病患者发病20年前即可发生变化,对相应区域的监测有利于对疾病发作进行更早的预测。
参考文献:
Altered iron and myelin in premanifest Huntington's Disease more than 20 years before clinical onset: Evidence from the cross-sectional HD Young Adult Study. https://doi.org/10.1016/j.ebiom.2021.103266
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#髓鞘#
33
#Lancet#
0
#铁代谢#
33
顶刊就是不一样,质量很高,内容精彩!学到很多
36