European Radiology:纳入这一参数的CCTA评分系统可实现PCI治疗效果的预测
2022-04-19 shaosai MedSci原创
经皮冠状动脉介入(PCI)目前,冠状动脉计算机断层扫描(CCTA)是经皮冠状动脉介入(PCI)术前评估操作难度最重要的手段。
 冠状动脉慢性完全闭塞(CTO)是一种常见的冠状动脉疾病,通过冠状动脉造影(CAG)可进行诊断。经皮冠状动脉介入(PCI)是治疗CTO(CTO-PCI)的主要手段。成功的CTO-PCI可以明显减轻心绞痛症状,改善左心室(LF)功能并提高长期生存率。然而,CTO-PCI在技术上比非闭塞性冠状动脉疾病的PCI更具挑战性,而且CTO-PCI后血管重建失败会增加出现不良后果的风险。因此,提高CTO-PCI的成功率对临床效益尤为重要。目前,冠状动脉计算机断层扫描(CCTA)是术前评估操作难度最重要的手段。
冠状动脉慢性完全闭塞(CTO)是一种常见的冠状动脉疾病,通过冠状动脉造影(CAG)可进行诊断。经皮冠状动脉介入(PCI)是治疗CTO(CTO-PCI)的主要手段。成功的CTO-PCI可以明显减轻心绞痛症状,改善左心室(LF)功能并提高长期生存率。然而,CTO-PCI在技术上比非闭塞性冠状动脉疾病的PCI更具挑战性,而且CTO-PCI后血管重建失败会增加出现不良后果的风险。因此,提高CTO-PCI的成功率对临床效益尤为重要。目前,冠状动脉计算机断层扫描(CCTA)是术前评估操作难度最重要的手段。
以往的病理研究显示,CTO段钙化和胶原纤维含量的增加与CTO-PCI治疗的时间有很好的相关性。纤维和钙化成分的增加增加了斑块的密度和硬度,这可能是导丝难以穿越闭塞段的组织学基础。最近,斑块分析软件的发展可进行定量分析,准确评估斑块的组织学特征。然而,目前CCTA的预测模型主要是基于病变部位的形态特征和肉眼估计的钙化斑块的严重程度,而在CTO段缺乏准确的斑块组织学的定性和定量指标。
近日,发表在European Radiology杂志的一项研究根据CCTA确定的临床、形态和组织学参数,建立了一个新的预测评分系统,为准确识别斑块成分提高CTO-PCI的成功率提供了技术支持。
本研究分析了来自两个中心的201名患者(平均年龄60.0[52.0-65.0]岁,85%为男性)的207个CTO病变的临床、形态和组织学特征。主要终点是导丝在30米内成功穿越病变。新的预测模型是由多变量分析确定的因素产生。包括斑块定量特征的CCTA斑块(CTAP)评分是通过给每个独立的预测因素分配一个适当的整数分数并将所有分数相加而产生的。此外,CTAP评分与其他基于CCTA的预测评分进行了比较。
63%的病变达到了终点。独立预测因素包括既往CTO-PCI失败、近端钝性残端、近端侧支、远端侧支、闭塞段弯曲>45°,以及高密度斑块体积(纤维体积+钙化体积)≥19.9 mm3。随着评分从0到5的增加,导丝在30米内穿越的成功率从96%降至0%。将CTAP评分与其他预测评分相比较,CTAP评分显示出最高的判别力(c统计量=0.81与0.73-0.77,p值0.02-0.07)。CTAP评分对程序性成功显示出相似的结果。
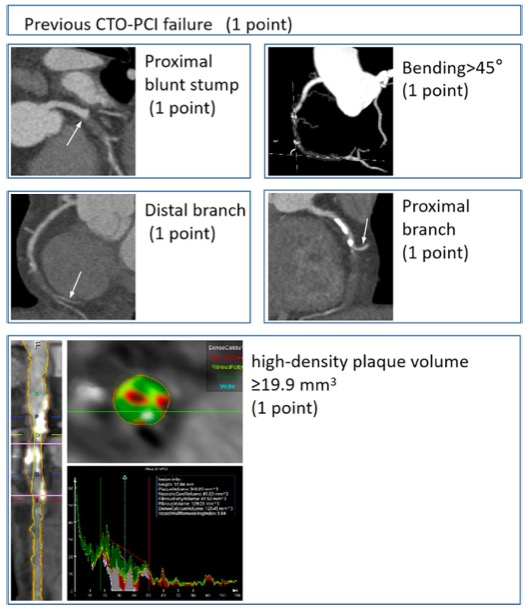
图 CTAP评分汇总
本研究表明,包括高密度斑块体积的预测模型可提高总体的预测能力,可有效地预测导丝穿越效率,并实现手术成功与否的准确预测。
原文出处:
Rui Wang,Yi He,Haoran Xing,et al.Inclusion of quantitative high-density plaque in coronary computed tomographic score system to predict the time of guidewire crossing chronic total occlusion.DOI:10.1007/s00330-022-08564-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
31
#CTA#
30
#治疗效果#
41
#PCI治疗#
45
#CCT#
0
认真***
57
#学习#😂
55