Nutrients:近年来绝经后乳腺癌患者化疗期间的代谢变化
2021-08-24 MedSci原创 MedSci原创
乳腺癌患者越来越重视体力活动和营养,因此代谢变化得到了较为明显的改善。
乳腺癌(BC)的治疗在过去几十年中稳步改善。尽管每年乳腺癌病例越来越多,但总体患者生存率正在上升,这主要是由于筛查计划和治疗的改进。目前,该病各个阶段的全球5年生存率为73%,发达国家和较低阶段的存活率均较高。
据统计,乳腺癌约占所有女性新发癌症的25%,相当于存在相当数量的长期乳腺癌幸存者。考虑到这一积极变化,必须进一步研究肿瘤治疗的长期后果。这反过来可以让临床医生更好地了解谁需要更密切地观察,并有助于抵消治疗可能产生的负面影响。
近半个世纪以来,人们一直认为接受辅助化疗的妇女代谢受损。这主要表现为平均体重增加3-5千克,但个体患者之间差异很大。这种负面变化的具体机制尚未完全阐明。同时,大多数激素受体阳性的早期BC患者会接受芳香化酶抑制剂,后者会进一步恶化代谢状况,特别是脂质状况。
在研究BC患者时,饮食和锻炼一直是人们越来越感兴趣的领域。因此,在检查代谢、疼痛和疲劳时,关注这些方面很重要,对于该患者,报告的结果(PROs)通常是选择的方法。患者报告的结果已被证明具有预后价值。
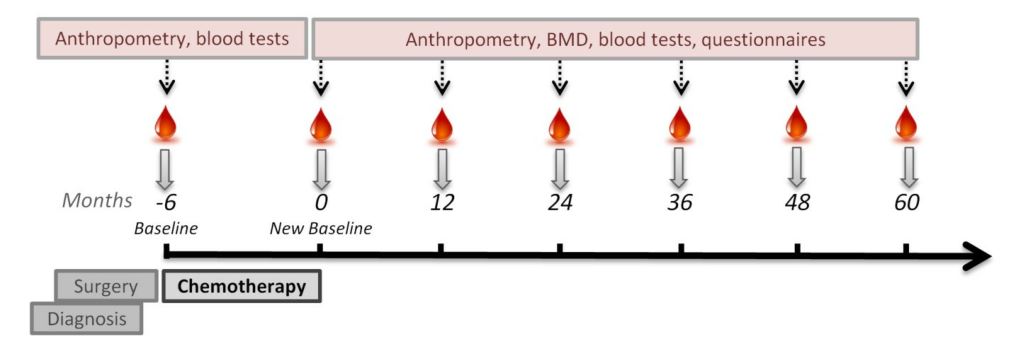
为了评估BC患者化疗期间体重增加的情况,来自丹麦哥本哈根大学呢分泌与代谢学组的专家对一组正在进行的前瞻性早期乳腺癌妇女队列进行了中期分析,结果发表在近期《营养学》Nutrients杂志上。同时,为了帮助解开体重变化的许多可能原因,研究人员还对患者血液检查、患者报告结果(PROs)和骨密度(BMD)进行了全面分析。
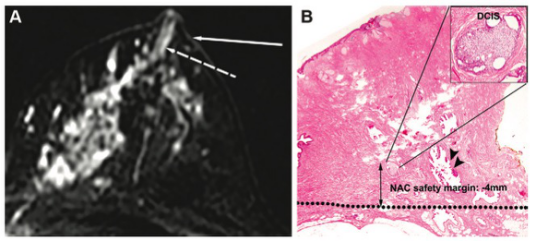
本研究纳入的38名患者均被诊断为BC,并接受化疗。大多数患者表现为浸润性导管癌(86.8%)和肿瘤2期(52.6%)或3期(38.8%)。大多数患者接受肿瘤切除术(63.2%),所有患者均接受紫杉醇治疗,大多数患者在治疗前接受环磷酰胺治疗(86.8%)。
试验设计
结果显示,所有患者接受化疗后平均体重增加了1.2公斤,但治疗前后体重没有显著性差异。除此之外,高密度脂蛋白胆固醇(HDL)显著下降,甘油三酯增加,胰岛素敏感性降低的趋势不明显。
研究人员发现,尽管化疗后女性报道了疼痛和疲劳程度增加,但她们的活动水平更高。而身体活动与长期BC幸存者健康相关生活质量的提高有关。此外,先前的研究表明,体力活动有助于保持骨密度和肌肉骨骼健康,而本研究发现根据年龄,BMD处于预期水平。
随访期间各项代谢指标变化
关于饮食摄入,BC患者饮食相对低脂,经常摄入蔬菜等纤维和高质量蛋白质。其他研究中也报道了这种饮食可能对患者有益。从2020年开始的系统回顾表明,应推荐低脂饮食和健康优质饮食,但癌症患者的饮食中不应排除任何食品类别(肉类、乳制品)。
总而言之,乳腺癌患者越来越重视体力活动和营养,因此代谢变化得到了较为明显的改善。
参考文献:
Weight Change in Post-Menopausal Women with Breast Cancer during Chemotherapy—Perspectives on Nutrition, Activity and Bone Metabolism: An Interim Analysis of a 5-Year Prospective Cohort. Nutrients 2021, 13(8), 2902; https://doi.org/10.3390/nu13082902
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#代谢变化#
31
#绝经#
29
#乳腺癌患者#
39
#绝经后#
30
学习了
55
学习
46
#学习#
57
#肿瘤#
56