JAHA:动脉粥样硬化疾病患者PCSK9抑制剂使用情况
2021-04-27 MedSci原创 MedSci原创
尽管有越来越多的疗效试验证据,指南建议在高风险ASCVD患者中使用PCSK9抑制剂,但从2015年到2019年,很少有患者开始使用PCSK9抑制剂。
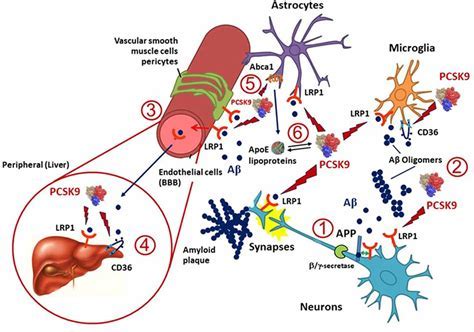
前蛋白转化酶枯草溶菌素9(PCSK9)抑制剂是一种有前景的降脂药物,尽管其使用受到成本方面的限制。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,这项回顾性队列研究使用了全国商业索赔数据库,该数据库纳入了年龄在18至64岁之间的动脉粥样硬化性心血管疾病(ASCVD)患者。
研究人员确定了从2015年第3季度到2019年第2季度美国食品药品管理局批准开始使用PCSK9抑制剂的ASCVD患者的数量。该研究的次要目标是明确在各种ASCVD风险组中使用PCSK9抑制剂的患者比例,他们根据他汀类药物使用情况和基线低密度脂蛋白胆固醇水平进行风险分层。
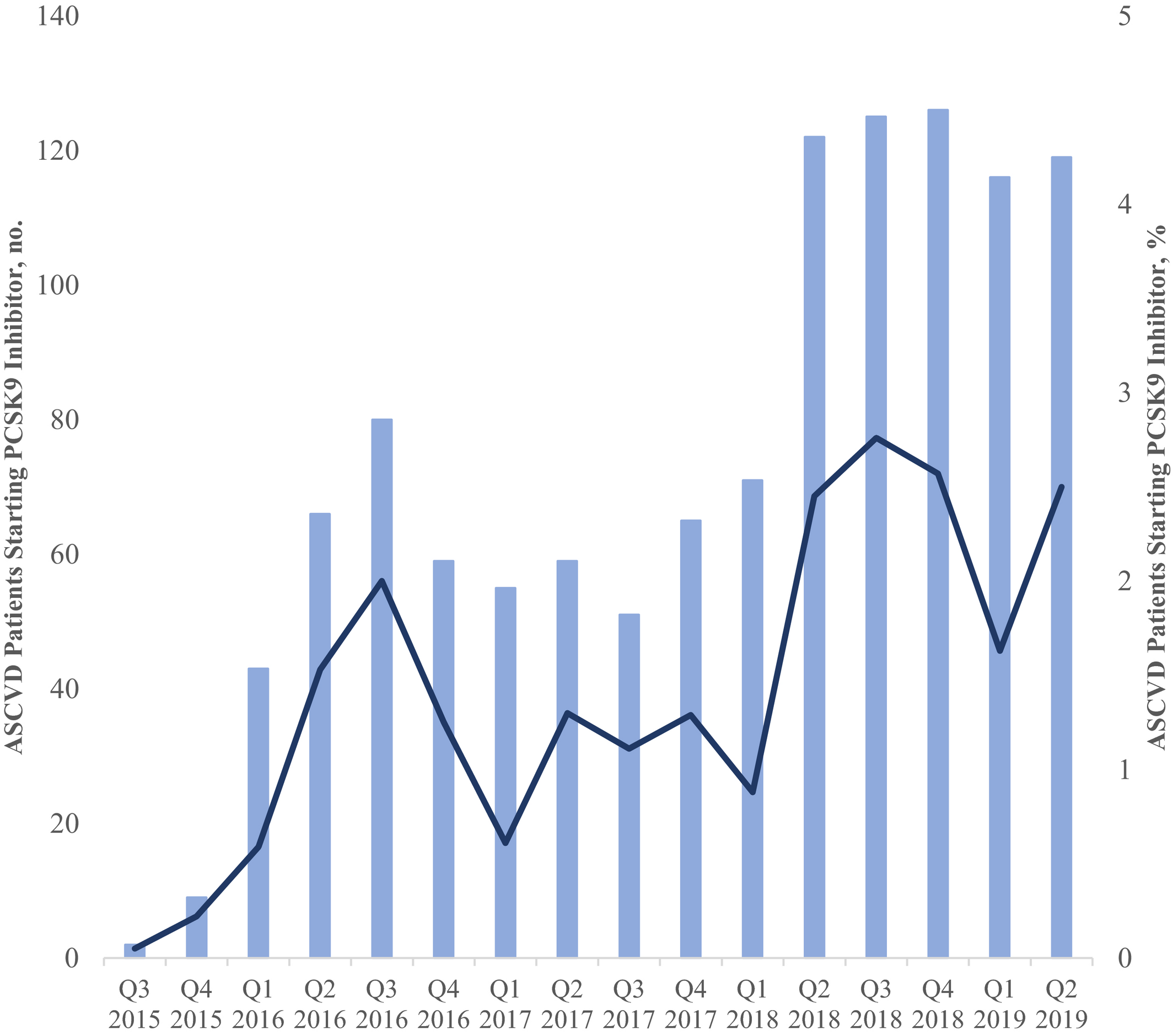
研究人员确定了126419例接受PCSK9抑制剂或他汀类药物治疗的ASCVD患者。在这些患者中,有1168名(0.9%)患者接受了PCSK9抑制剂治疗。接受PCSK9抑制剂治疗的患者人数从2015年第3季度的2名患者增加到2019年第2季度的119名患者,相当于已经接受他汀类药物治疗的患者开始使用PCSK9抑制剂治疗的比例从0.05%增至2.5%。在对高强度他汀类药物高度依从的ASCVD患者中,13643例患者低密度脂蛋白胆固醇≥70 mg/dL,在这一亚组中,119例(0.9%)患者开始使用PCSK9抑制剂治疗。
由此可见,尽管有越来越多的疗效试验证据,指南建议在高风险ASCVD患者中使用PCSK9抑制剂,但从2015年到2019年,很少有患者开始使用PCSK9抑制剂。价格下降的幅度可能还不足以影响PCSK9抑制剂的使用。
原始出处:
Elias J. Dayoub.et al.Adoption of PCSK9 Inhibitors Among Patients With Atherosclerotic Disease.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.019331
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#PCSK9抑制剂#
52
#PCSK9抑制#
36
#抑制剂#
33
#疾病患者#
27
#使用情况#
37
#PCS#
32
#Csk#
29
#粥样硬化#
29
#AHA#
24
有帮助
60