UCB在《Lancet》上发表bimekizumab治疗斑块状银屑病的全新数据
2021-02-08 Allan MedSci原创
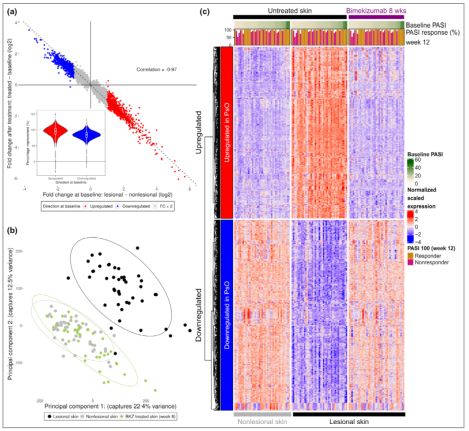
《Lancet》杂志发表了两项研究性治疗药物bimekizumab治疗中度至重度斑块状银屑病III期研究。来自BE VIVID和BE READY研究的数据表明,
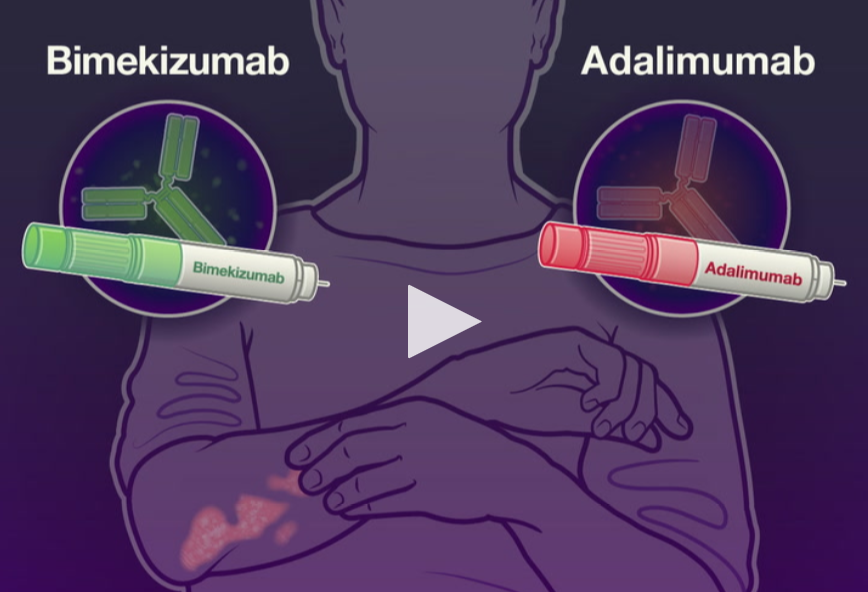
《Lancet》杂志发表了两项研究性治疗药物bimekizumab治疗中度至重度斑块状银屑病III期研究。来自BE VIVID和BE READY研究的数据表明,与接受安慰剂或强生的Stelara(ustekinumab)治疗的患者相比,接受bimekizumab治疗的患者在第16周的皮肤清除水平更高。两项研究均以银屑病面积和严重程度指数(PASI 90)和研究者全局评估指数(IGA)至少改善90%来衡量。
UCB已向美国食品药品监督管理局(FDA)和欧洲药品管理局(EMA)提交营销申请。FDA和EMA分别于2020年9月接受了该公司针对中度至重度斑块状银屑病的bimekizumab的生物制剂许可申请(BLA)和市场许可申请(MAA)。
银屑病斑块的产生是由于皮肤细胞以异常高的速率生长。这种快速细胞生长的原因是未知的,但免疫系统的问题被认为发挥了一定的作用。这种疾病往往在家庭中流行,某些基因与银屑病是相关的。
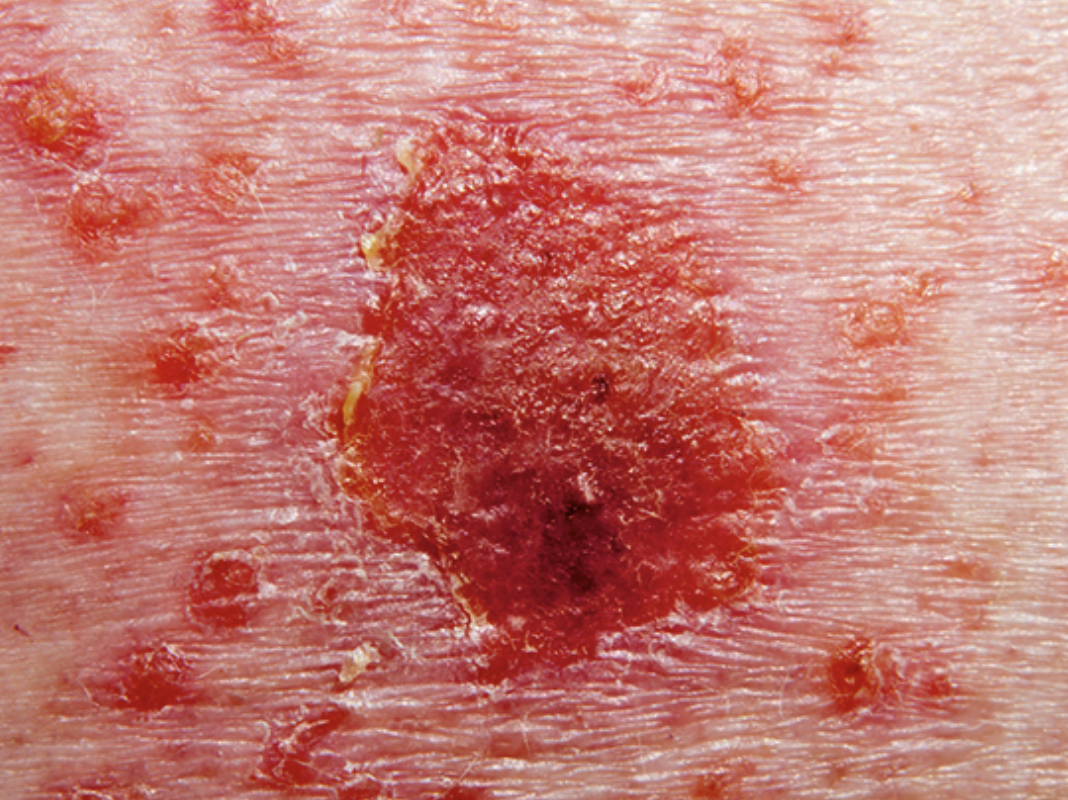
斑块状银屑病(最常见的银屑病类型)通常在发作之初表现为头皮、肘部、膝盖、背部或臀部有一块或多块红色、银色、有光泽的小斑片(斑块)。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#MEK#
36
#mAb#
28
#Lancet#
30
#斑块#
57
#斑块状银屑病#
66
#UCB#
43
顶刊就是不一样,质量很高,内容精彩!学到很多
57