Gastroenterology:强化肠内营养并不能改善重型酒精性肝炎患者生存期
2016-01-26 Mechront 译 MedSci原创
重型酒精性肝炎(AH)是一种危及生命的疾病,该疾病的治疗需要有足够的口服营养支持。研究者进行了一项随机对照试验,探究重型AH的治疗里使用强化的肠内营养能否改善疗效。该研究共纳入了136名18-75岁重度饮酒者,近期出现黄疸表现,且活组织病检确诊为重型AH的患者。按1:1随机分为以下两种治疗方案组:强化的肠内营养+甲基强的松龙(试验组)、传统的营养+甲基强的松龙(对照组)。强化的肠内营养患者通过鼻胃
重度酒精性肝炎(AH)是一种危及生命的疾病,该疾病的治疗需要有足够的口服营养支持。研究者进行了一项随机对照试验,探究重度AH的治疗中使用强化的肠内营养能否改善疗效。
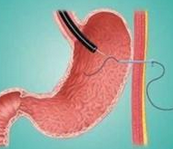
该研究共纳入了136名18-75岁重度饮酒者,近期出现黄疸表现,且活组织病检确诊为重度AH的患者。按1:1随机分为以下两种治疗方案组:强化的肠内营养+甲基强的松龙(试验组)、传统的营养+甲基强的松龙(对照组)。强化的肠内营养患者通过鼻胃管予以肠内营养14天。该研究以患者6个月的生存作为主要结局指标。
研究结果显示,试验组和对照组6个月时间里的累积死亡率分别为44.4%(95% CI, 32.2%-55.9%)和52.1% (95% CI, 39.4%-63.4%),ITT分析后并没有发现两组间死亡率差异(P=.406)。试验组有48.5%的患者提前结束鼻胃管予以肠内营养阶段,有5名患者发生了与肠内营养相关的严重不良事件。不管是试验组还是对照组,均表现出更大比例的患者群体每日卡路里摄入<21.5 kcal/kg(65.8%; 95% CI, 48.8-78.4),每日卡路里摄入更高的患者群体占33.1%(95% CI, 23.1%- 43.4%) (P<.001)。
研究结果表明,强化的肠内营养不仅依从性不好,难以实现,并且也不会增加患者生存期;不管哪种营养方式,每日能量摄入不够仍是个大问题,会导致更高的死亡率,因此足够的营养摄入量仍是重型AH治疗的主要目标之一。
原始出处:
Moreno C, Deltenre P,et al.Intensive Enteral Nutrition is Ineffective for Individuals with Severe Alcoholic Hepatitis Treated with Corticosteroids.Gastroenterology. 2016 Jan 4.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Gastroenterol#
23
#AST#
28
#肝炎患者#
29
#酒精性#
26
#GAS#
36
#患者生存#
34
有用
103
是的
122
#生存期#
34
#Gastroenterology#
28