Cardiovasc Diabetol :糖尿病-心-肾疾病的流行病学:一项140万成人的横断面研究
2022-07-08 从医路漫漫 MedSci原创
2型糖尿病会导致心力衰竭和慢性肾病,心力衰竭会导致肾功能下降,反之亦然,是心肾综合征的一部分。

背景:在全球范围内,大约有5.37亿受试者患有2型糖尿病,6.97亿受试者患有慢性肾病(CKD),6400万受试者患有心力衰竭(HF) 。这些情况共同形成了恶性病理生理循环,其中一种情况的出现可能会促进其他情况的发展。例如,2型糖尿病会导致心力衰竭和慢性肾病,心力衰竭会导致肾功能下降,反之亦然,是心肾综合征的一部分。
几年来,2型糖尿病、慢性肾病和心力衰竭的治疗方案并不一定重叠。例如,噻唑烷二酮类药物有利于2型糖尿病患者的血糖控制;内皮素受体拮抗剂改善CKD患者的肾脏预后。然而,两者都与心力衰竭风险增加相关。肾素-血管紧张素-醛固酮系统阻断可改善心力衰竭或慢性肾病患者的预后,但不影响血糖控制。最近,钠-葡萄糖协同转运蛋白2抑制剂(SGLT2i)被证明可以改善2型糖尿病患者的血糖控制,减少心力衰竭和慢性肾脏病的发作,并改善慢性肾脏病或心力衰竭伴或不伴2型糖尿病患者的预后。因此,SGLT2i疗法使“糖尿病-心肾谱”(DCR谱)中的患者受益。尽管这些疾病的流行病学特征已有描述,但缺乏关于不同性别和年龄亚组DCR谱不同组成部分重叠的当代高质量流行病学数据。当评估特定患者具有一种或多种DCR频谱成分的概率时,这种证据差距转化为临床障碍。
目的:我们对在以色列马卡比医疗保健服务(MHS)注册的成年人进行了横断面分析。该数据库享有极高的年保留率(99%),经验证的2型糖尿病和心力衰竭登记,以及高粒度的估计肾小球滤过率(eGFR)测量。我们利用这些优势以高分辨率描述了当代(2019年)不同年龄和性别类别的DCR谱组成部分的患病率和重叠。
方法:这是一项对≥ 25岁成年人的横断面分析,于2019年在以色列大型医疗保健维护组织Maccabi Healthcare Services注册。收集的数据包括性别、年龄、T2D或心力衰竭的存在以及过去两年中最后一次估计的肾小球滤过率(eGFR)。T2D、心力衰竭或表皮生长因子受体< 60毫升/分钟/1.73平方米的受试者被定义为在糖尿病-心脏-肾脏(DCR)范围内。
结果:总共纳入了1,389,604名受试者(52.2%为女性);445,477人(32.1%)年龄在25至< 40岁,468,273人(33.7%)年龄在40至< 55岁,475,854人(34.2%)年龄≥ 55岁。74.7%的参与者和超过97%的T2D或心力衰竭患者可进行eGFR测量。eGFR的可用性在老年组中增加。有140,636名(10.1%)T2D患者,54,187名(3.9%)eGFR < 60mL/min/1.73 m2,11,605名(0.84%)心力衰竭患者。总的来说,12.6%的人至少有一种DCR症状,2.0%的人至少有两种,0.23%的人三种都有。心肾综合征(心力衰竭和表皮生长因子受体均< 60毫升/分钟/1.73平方米)在整个人群中占0.40%,在T2D患者中占2.3%。在同时患有心力衰竭和T2D的患者中,55.2%的患者eGFR < 60毫升/分钟/1.73平方米,15.8%的患者eGFR < 30毫升/分钟/1.73平方米。在DCR谱的患者中,T2D在年轻参与者中表现突出,但随着年龄的增长,逐渐被心力衰竭和eGFR < 60毫升/分钟/1.73平方米所取代。这三种情况的一致性随着年龄的增长而增加。
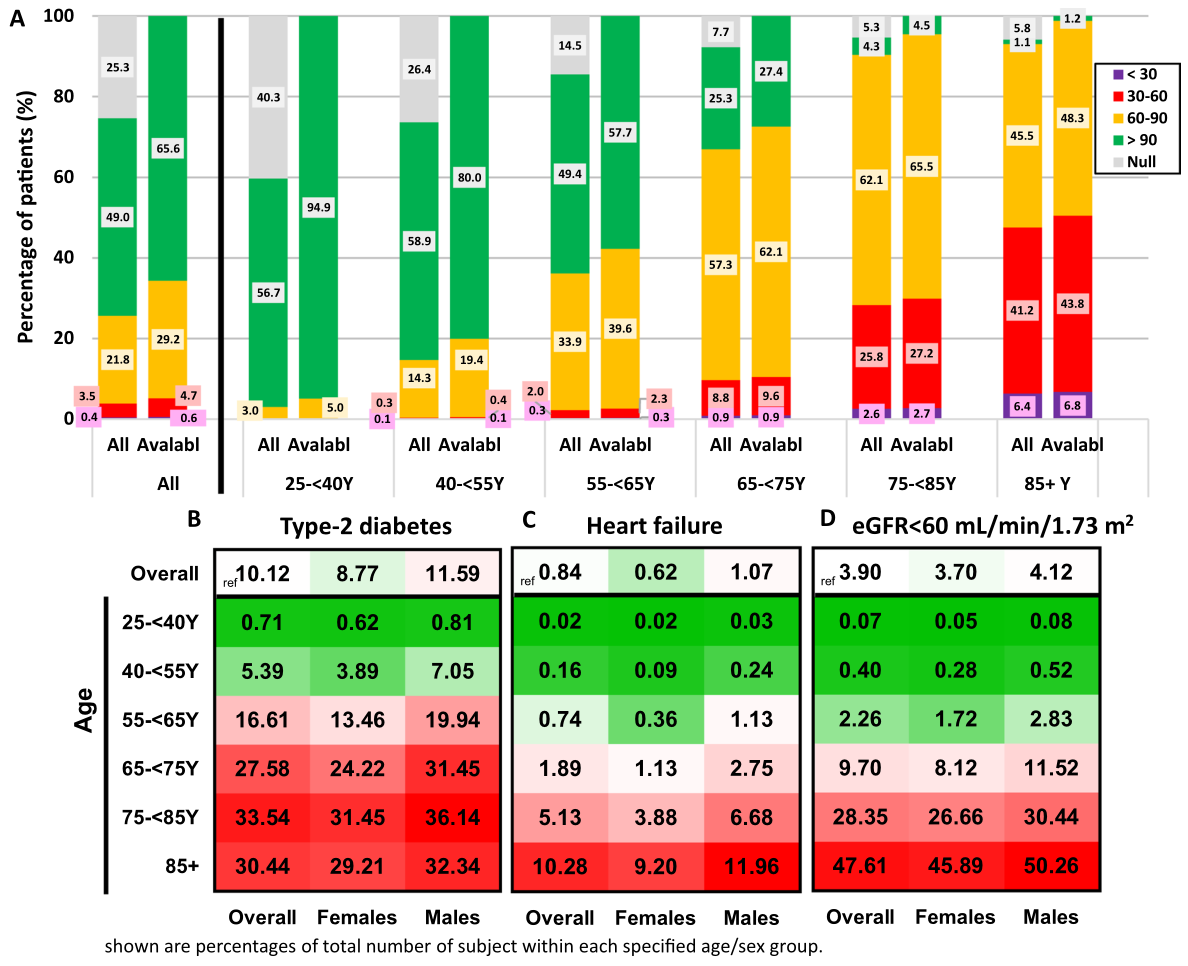
图1按年龄和性别划分的2型糖尿病、心力衰竭或肾功能减退(eGFR < 60 mL/min/1.73 m2)的患病率。MHS人群中各年龄组eGFR值的分布,表示为整个队列(all)的百分比和过去两年中eGFR值可用者的百分比(“可用”)。eGFR值表示为毫升/分钟/1.73平方米。b . T2D的流行率;C HF或D eGFR < 60毫升/分钟/1.73平方米,按年龄和性别分组。数字表示MHS数据库中患者在整个性别/年龄匹配人群中所占的百分比。对于每种情况,绿色表示患病率较低,红色表示患病率较高。白色表示研究人群中的总体患病率。T2D 2型糖尿病、心力衰竭、eGFR估计肾小球滤过率、MHS Maccabi医疗保健服务

图2按年龄组划分的糖尿病-心脏-肾脏(DCR)疾病谱的重叠部分。显示T2D(蓝色)、心力衰竭(黄色)和表皮生长因子受体(eGFR )< 60毫升/分钟/1.73平方米(绿色)患者分布及其一致性程度的比例文氏图,A表示总体人群,B表示年龄组。每个年龄组的面积与总人口成比例(根据DCR谱中的患者数量),例如,所有年龄组的“黄色/心力衰竭”面积之和大约等于总人口中的“黄色/心力衰竭”面积。经BioRender.com许可创建。T2D 2型糖尿病,心力衰竭,DCR糖尿病-心肾,eGFR估计肾小球滤过率
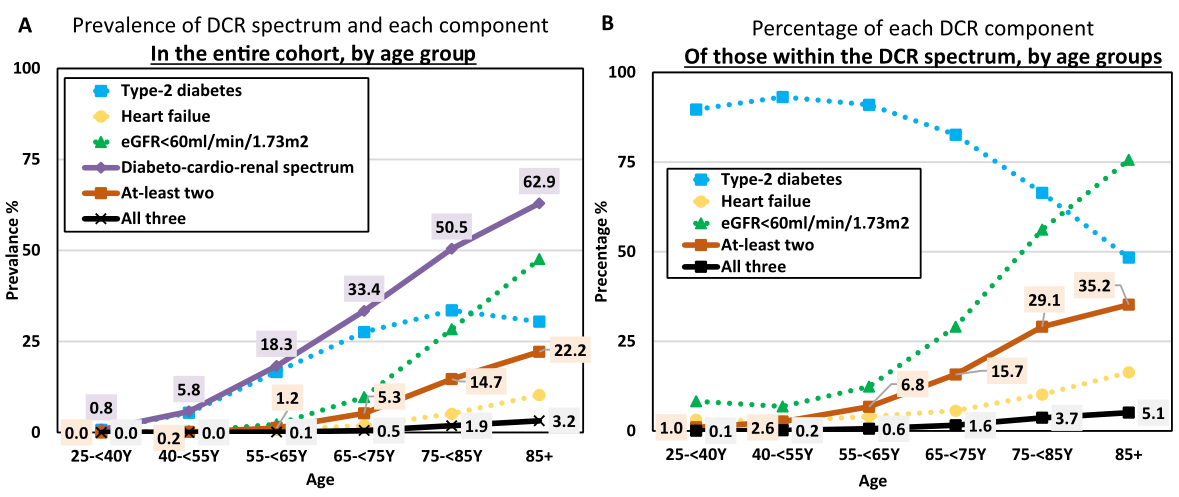
图3按年龄组划分的糖尿病-心-肾(DCR)谱及其组成部分的患病率。具有至少一种DCR谱成分(定义为T2D、心力衰竭或表皮生长因子受体< 60毫升/分钟/1.73平方米;紫色),在整个队列的受试者中,不同年龄组的患者具有至少两种(橙色)或所有三种(黑色)成分。b DCR谱不同组成部分的患病率(如A所示),特别是在DCR谱范围内(即T2D、心力衰竭和/或表皮生长因子受体< 60毫升/分钟/1.73平方米),按年龄组划分。T2D 2型糖尿病,心力衰竭,DCR糖尿病-心肾,eGFR估计肾小球滤过率
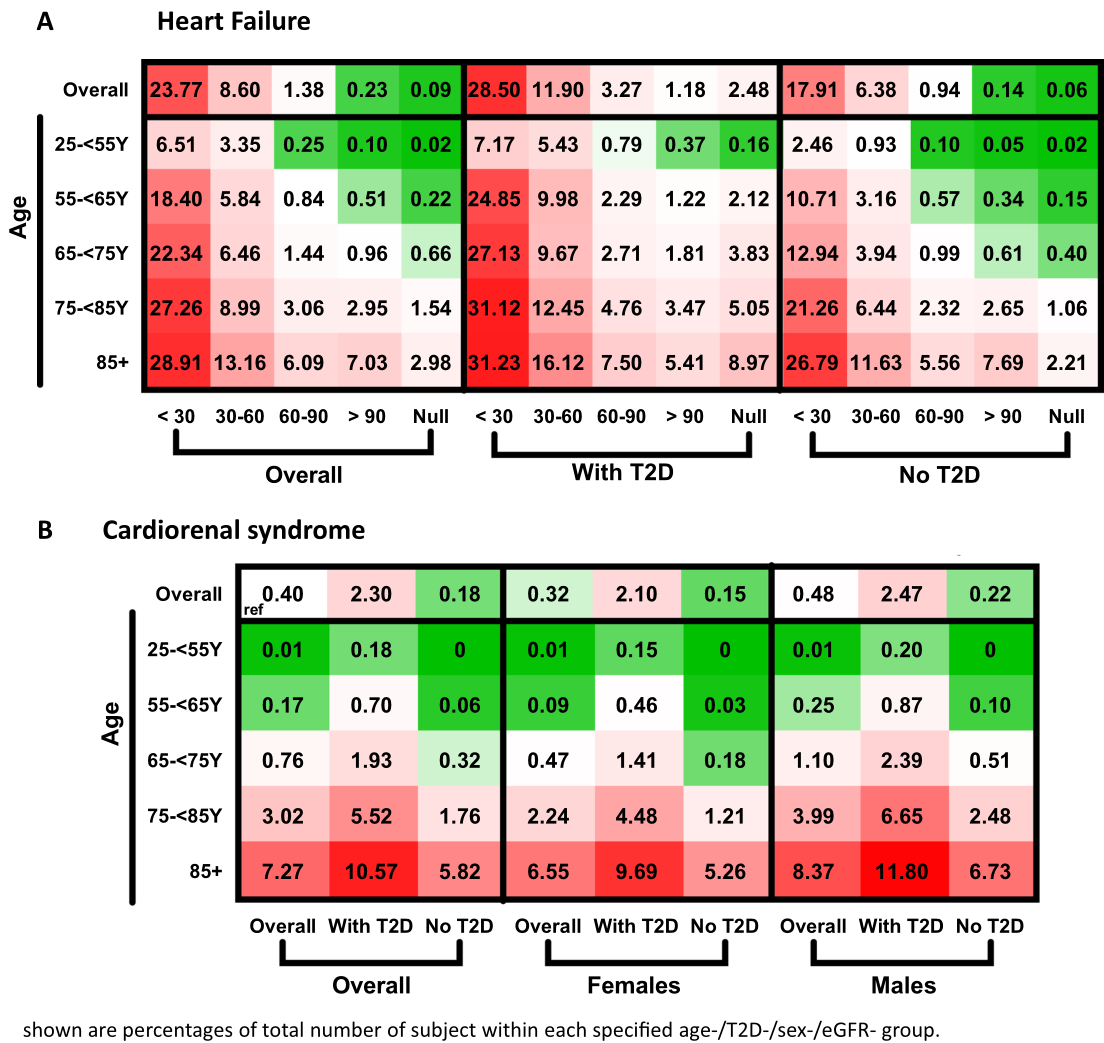
图4 2型糖尿病和肾功能对心力衰竭患病率的影响。根据年龄、T2D和表皮生长因子受体分类心力衰竭患病率。按年龄、性别和是否存在T2D分类的心肾综合征(定义为心力衰竭和eGFR < 60 ml/min/1.73 m2)的患病率。数字表示MHS中患者占整个性别/年龄/T2D/eGFR类别匹配人群的百分比。绿色表示患病率较低,红色表示患病率较高。白色(参照)代表研究人群中的总体患病率(心力衰竭为0.84%,心肾综合征为0.40%)。eGFR类别以毫升/分钟/1.73平方米为单位。T2D 2型糖尿病,eGFR估计肾小球滤过率,MHS马卡比医疗保健服务
结论:这项大规模、基础广泛的研究提供了当代高分辨率的DCR频谱及其组成部分的患病率。该结果强调了不同年龄T2D、心力衰竭和肾功能不全之间的优势和一致性程度的差异。
原文出处:Schechter M, Melzer Cohen C, Yanuv I,et al.Epidemiology of the diabetes-cardio-renal spectrum: a cross-sectional report of 1.4 million adults.Cardiovasc Diabetol 2022 Jun 10;21(1)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#横断面#
60
#ASC#
38
#BET#
30
#DIA#
30
#流行病#
36