CID:马拉韦罗在HIV-1感染孕妇体内的药代动力学变化
2021-09-25 从医路漫漫 MedSci原创
马拉韦罗是C-C趋化因子受体5 (CCR5)的拮抗剂,在阻止HIV-1进入易感细胞中起重要作用。作为cART治疗的一部分,对CCR5-tropic HIV-1有效。
马拉韦罗是C-C趋化因子受体5 (CCR5)的拮抗剂,在阻止HIV-1进入易感细胞中起重要作用。作为cART治疗的一部分,对CCR5-tropic HIV-1有效。成人或青少年马拉韦洛治疗的标准推荐剂量为300mg,每日两次,在同时给予增强蛋白酶抑制剂时剂量可以减少到150mg,每日两次。目前尚无资料描述妊娠期间使用马拉韦洛克的药代动力学和安全性,美国卫生与公众服务部的围产期指南也没有关于妊娠期间马拉韦洛克治疗或给药方案的建议
目的:描述马拉韦罗在妊娠和产后感染人类免疫缺陷病毒(HIV)的妇女体内的药代动力学。
方法:接受马拉韦洛克治疗的HIV感染孕妇在妊娠晚期和分娩后≥2周进行了强化的稳态12小时药动学分析。在分娩时采集脐带血样本和匹配的母亲血液样本。这些数据是在两项研究中收集的:P1026(美国)和Panna(欧洲)。计算药代动力学参数。
结果:18名女性被纳入分析。大多数女性(12名;67%)每天服用150mg的马拉韦罗加蛋白酶抑制剂,2名(11%)的女性每天服用300mg不加蛋白酶抑制剂,4名(22%)接受替代方案。妊娠晚期和产后马拉韦罗的几何平均比率分别为0.72(90%可信区间,0.60-0.88)和0.70(0.58-0.85)。只有1名患者在孕期和产后的血药低谷浓度低于建议的50 ng/mL目标。马拉韦罗脐带血与母亲血液的比值中位数为0.33(范围为0.03-0.56)。接近分娩时病毒载量<50拷贝/毫升的有13例(76%)。所有儿童在检测时均为HIV阴性。
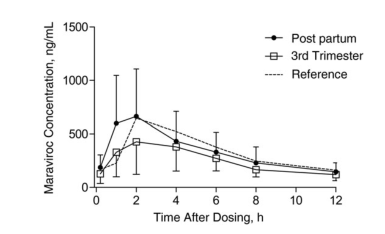
图1 马拉韦罗(含蛋白酶抑制剂,每天两次,150mg)在妊娠(妊娠晚期)和产后的平均浓度-时间曲线。数值代表稳态的平均马拉韦罗浓度(带有标准偏差)。
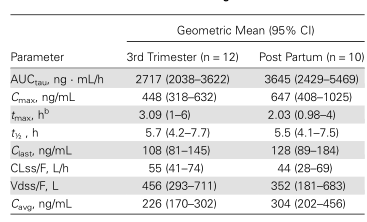
表1 马拉韦罗标准方案孕期和产后的药代动力学参数
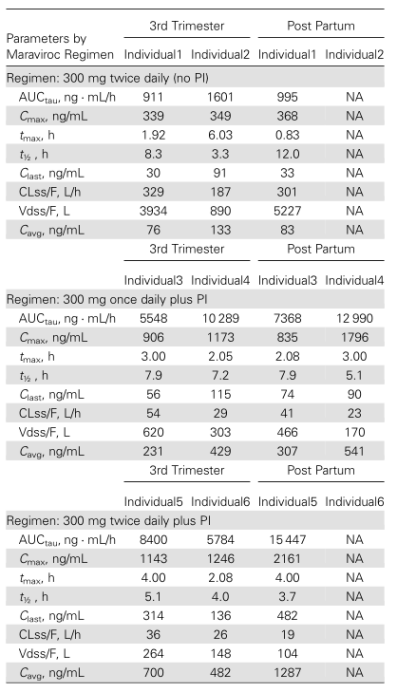
表2 不同马拉韦罗方案孕期和产后的药代动力学参数
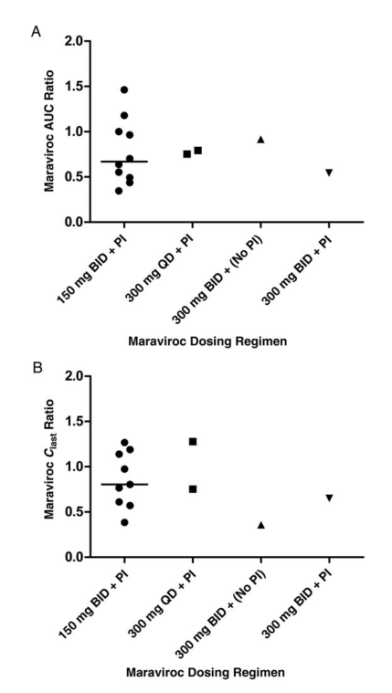
图2 按给药方案测定妊娠晚期与产后马拉韦ROC曲线下面积(AUC) (A)最后时间点浓度(Clast) (B)个体比值。对于150mg方案,中位数显示(线)。缩略语:BID,每日两次;π,蛋白酶抑制剂;QD,每天一次。
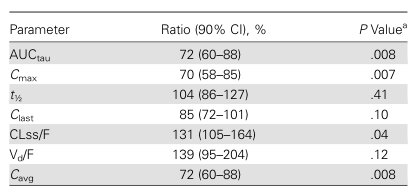
表3 马拉韦ROC药代动力学的几何平均比值:妊娠晚期与产后(n = 14)
结论:妊娠期马拉韦罗的总体暴露减少,AUCtau降低,最高浓度约为30%,Ctragh值降低了15%,但超过了目标浓度下限。因此,在怀孕期间服用标准成人剂量似乎足够了。
原文出处
Colbers A, Best B, Schalkwijk S,et al,Maraviroc Pharmacokinetics in HIV-1-Infected Pregnant Women.Clin Infect Dis 2015 Nov 15;61(10)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#药代#
53
#CID#
59
#药代动力学#
56
学习充电
77