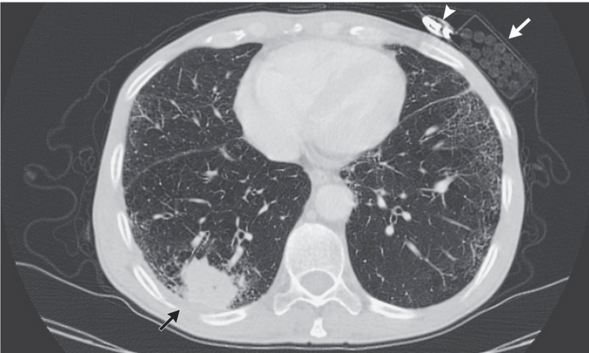
CLIN CANCER RES:PI3K和CDK4/6联合抑制治疗PIK3CA突变肺鳞状细胞癌
2018-12-19 MedSci MedSci原创
肺鳞状细胞癌(LUSC)是非小细胞肺癌的主要亚型,其特征是存在多种遗传改变,特别PI3K通路改变,在超过50%的LUSC病例中得到证实。尽管是具有治疗前景的靶点,单一药物PI3K抑制剂在LUSC中表现的治疗效果一般。因此需要靶向LUSC的新型组合疗法。CLIN CANCER RES近期发表了一篇文章研究这一问题。
肺鳞状细胞癌(LUSC)是非小细胞肺癌的主要亚型,其特征是存在多种遗传改变,特别PI3K通路改变,在超过50%的LUSC病例中得到证实。尽管是具有治疗前景的靶点,单一药物PI3K抑制剂在LUSC中表现的治疗效果一般。因此需要靶向LUSC的新型组合疗法。CLIN CANCER RES近期发表了一篇文章研究这一问题。
作者在LUSC患者的异种移植模型(PDX)中评估PI3K抑制剂单独和与CDK4/6抑制剂联合的治疗效果。还进行了药效学研究以确认化合物的靶向抑制效果。研究结果表明,与LUSC的癌症基因组图谱分析的结果一致,研究中的LUSC PDX模型基因组谱分析发现超过50%的模型中存在PI3K通路改变。在12模型中使用PI3K抑制剂发现PIK3CA突变鉴定是治疗反应的预测标志。与单药治疗相比,在PIK3CA突变的模型中使用PI3K和CDK4/6的联合抑制抗肿瘤效果更明显。此外,两种药物的组合可以达到对PI3K和细胞周期途径的靶向抑制。
原始出处:
Ruoshi Shi, Ming Li, et al. Targeting the CDK4/6-Rb Pathway Enhances Response to PI3K Inhibition in PIK3CA-Mutant Lung Squamous Cell Carcinoma. CLIN CANCER RES. December 2018 doi: 10.1158/1078-0432.CCR-18-0717
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
36
#PIK3CA#
32
#CDK4#
29
#PIK3CA突变#
24
#肺鳞状细胞癌#
26
#PI3K#
28
#CDK#
29
#CDK4/6#
29