Ear Nose Throat J:慢性中耳炎患者听力恢复预后模型的开发和验证
2022-01-08 AlexYang MedSci原创
调查了影响慢性中耳炎(COM)患者术后听力恢复的因素,建立了听力恢复的临床预测模型,并验证了该模型的准确性。
慢性中耳炎(COM)通常影响到不同年龄、性别和地区的人。中耳炎的具体风险因素包括与个体有关的因素和环境因素,如过敏、免疫抑制、上呼吸道感染和社会经济地位。在一些发展中国家,COM的发病率大于4%;然而,在美国,发病率小于1%。

最近,来自山东大学齐鲁医学院的研究人员在《Ear Nose Throat J》上发表文章,调查了影响慢性中耳炎(COM)患者术后听力恢复的因素,建立了听力恢复的临床预测模型,并验证了该模型的准确性。
研究人员对2012年1月1日至2020年9月30日期间收治的COM患者数据进行了回顾性分析。收集了患者相关的临床病理特征数据。患者随机分为开发队列和验证队列。术后气骨间隙(ABG)≤20分贝定义为听力恢复成功。单变量和多变量的逻辑回归分析用来调查几个预后因素与听力恢复的关系。这些因素随后用于建立一个诺模图。利用自举法进行了模型内部验证,并在分辨力、校准和临床有效性方面进行了性能评估。
研究包括2146名COM患者:开发队列包括1610名患者(平均[标准差;SD]年龄,44.1[14.7]岁;733名男性[45.5%]),验证队列包括536名患者(平均[SD]年龄,42.9[14.4]岁;234名男性[43.7%])。多变量逻辑回归分析显示,年龄、发病时间、手术方式(鼓室成形术、管壁向上-CWU或管壁向下-CWD)、听骨假体、听骨链周围的肉芽或钙化块、听骨链完整性、钻孔时间、咽鼓管功能障碍、混合性听力损失、半规管瘘管和二次手术都与听力恢复有关。基于这些变量构建了一个诺模图。曲线下面积在发展队列中是0.797(95%置信区间[CI],0.778-0.812),在验证队列中是0.798(95%CI,0.7605-0.8355)。
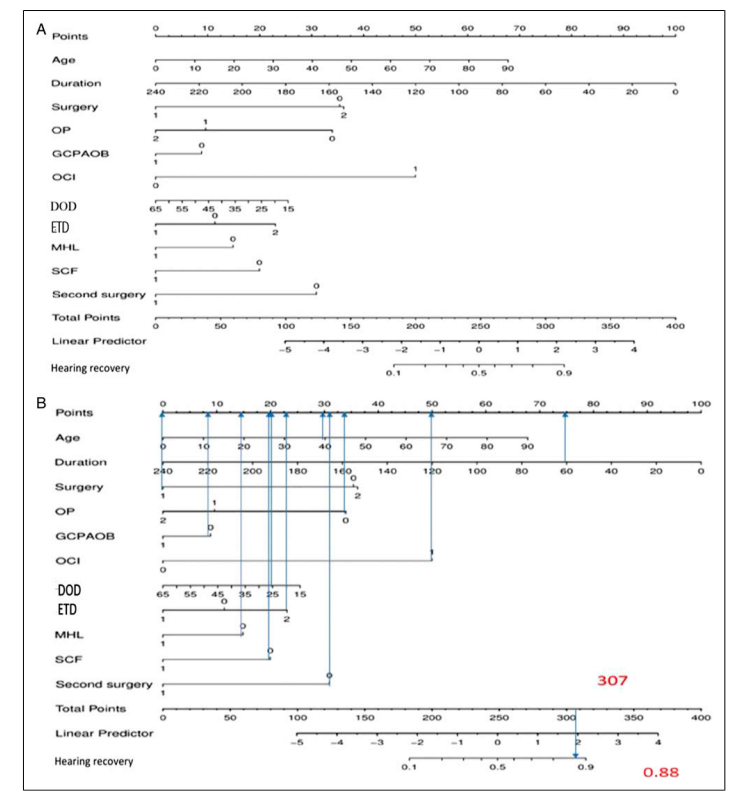
开发的预后诺模图
综上所述,很多临床因素与COM患者的听力恢复相关。利用这些数据开发的诺模图可以提供个性化的听力恢复风险评估,助力术前咨询,并有助于为患者设定现实的期望。
原始出处:
Fengyang Xie , Xiaoyue Zhen , Haiyuan Zhu et al. Development and Validation of a Prognostic Model to Predict Hearing Recovery for Patients With Chronic Otitis Media. Ear Nose Throat J. Dec 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习了
42
#OAT#
38
#听力#
57
#中耳炎#
40