Nat Commun:母体孕前维生素D状况影响后代性别比例
2021-05-16 haibei MedSci原创
最近的一项研究结果显示,在1228名试图怀孕的妇女中,孕前25-羟维生素D的浓度与活产男婴呈正相关,在高敏C反应蛋白(一种系统性低度炎症的标志物)升高的妇女中,该相关性明显增强。
根据进化理论,一些动物物种可以根据母体健康状况和资源可用性调整其后代性别比例,这种能力赋予了自然选择优势,在一些不利的情况下,雌性不太可能生育雄性后代。在过去的几十年里,在北美、欧洲和亚洲,人们已经观察到人类的男女性别比明显下降。尽管影响这种转变的因素尚不清楚,但有几条证据表明,母体炎症可能对男性胚胎的植入或存活有害,这可能有助于人口规模上的性别比下降。
事实上,研究人员以前在阿司匹林对妊娠和生殖的影响[EAGeR]试验中证明,孕前启动的低剂量阿司匹林(LDA)给药可恢复炎症高发妇女出生时的性别比下降,这表明这种现象也可能发生在人类身上。
在观察性研究中,暴露于吸烟、甲基汞和地震同样与性别比下降有关,这进一步表明,特定人群中男女活产的比例可能对一系列环境压力因素敏感,这可能通过炎症途径调节。生态学数据还表明,在世界一些地区存在着季节性、海拔和纬度性的性别比梯度,在纬度较高、海拔较低和低温时期,男性活产率降低,这意味着维生素D的潜在作用,维生素D在阳光照射期间在表皮内合成。

但是,目前为止,关于维生素D的状态是否与后代的性别比有关,我们还不清楚。最近的一项研究结果显示,在1228名试图怀孕的妇女中,孕前25-羟维生素D的浓度与活产男婴呈正相关,在高敏C反应蛋白(一种系统性低度炎症的标志物)升高的妇女中,该相关性明显增强。
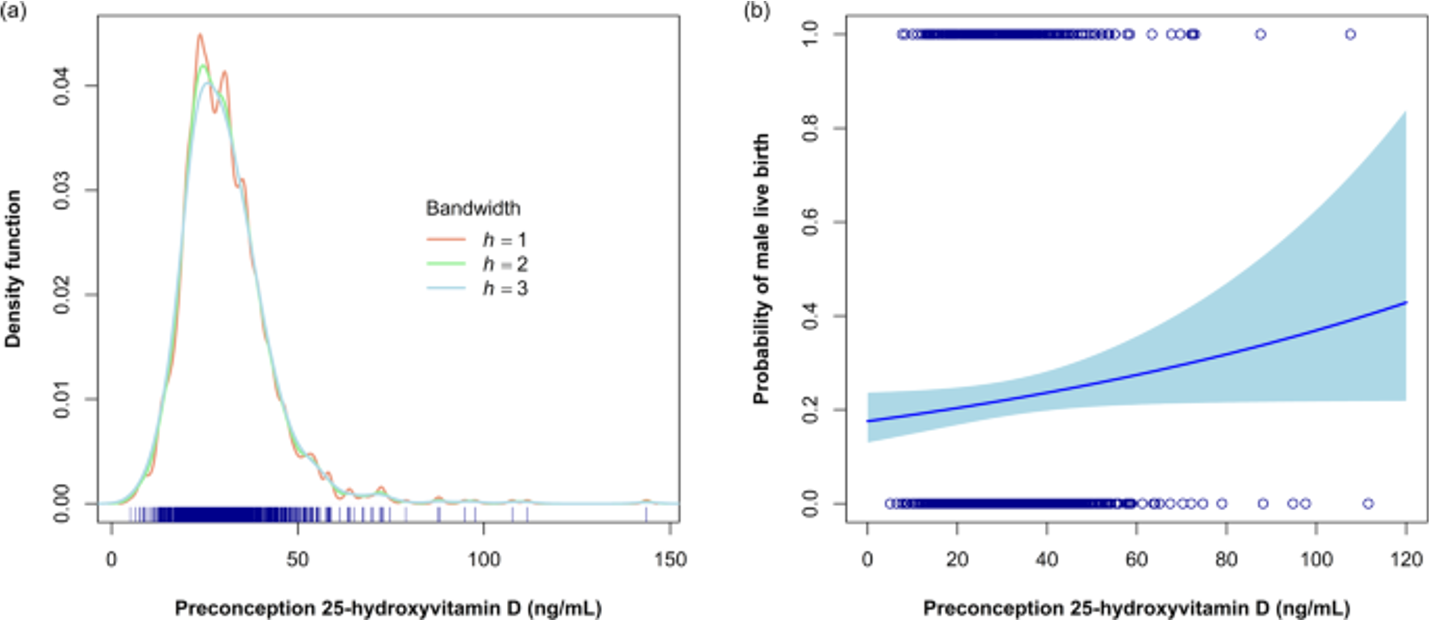
孕前25-羟基维生素D[25(OH)D]水平的分布及其与男胎活产的关系
该研究结果表明,维生素D可以减轻母体的炎症,否则将不利于男性胎儿在子宫内的植入或生存。
原始出处:
Alexandra C. Purdue-Smithe et al. The role of maternal preconception vitamin D status in human offspring sex ratio. Nature Communications (2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













有意思
30
#孕前#
32
#COMMUN#
26
#Nat#
22
这将是个有用的信息吗
68