Neurocrit Care:脑室外引流导管通道出血
2018-09-28 杨中华 脑血管病及重症文献导读
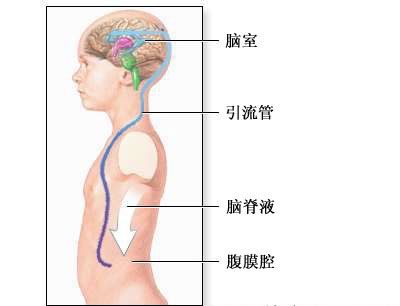
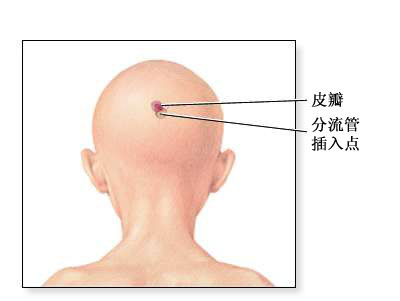
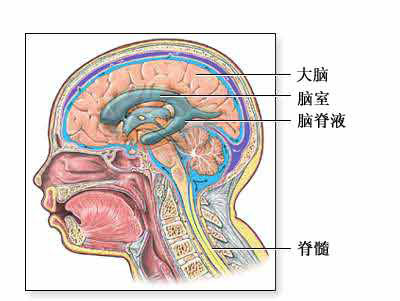
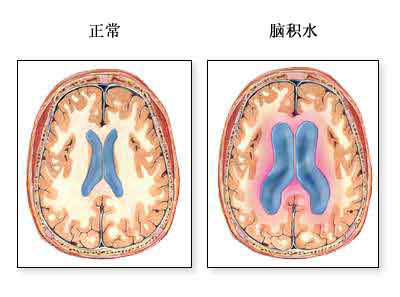
脑室外引流(external ventricular drain,EVD)最常见的适应症为监测和控制创伤性脑损伤、急性脑积水、脑室出血和SAH。EVD最常见的并发症为出血和感染。
脑室外引流(external ventricular drain,EVD)最常见的适应症为监测和控制创伤性脑损伤、急性脑积水、脑室出血和SAH。EVD最常见的并发症为出血和感染。相对于感染,导管通道出血(catheter tract hemorrhage,CTH)一般不太受到关注。脑室造口的新发出血或血肿扩大的比例为0.7% - 41%。Dey等系统性综述显示不同研究EVD出血的风险差异很大,出血的定义没有标准化。年龄>75岁,INR>1.4,使用抗栓药物等是CTH的危险因素。
CLEAR III试验是一项随机双盲多中心III期临床试验,纳入了500例脑室出血患者,评价了阿替普酶通过EVD脑室内注入阿替普酶的有效性。2018年8月来自美国的Achim Mu¨ ller等在Neurocritical Care上公布了他们的研究结果,他们利用CLEAR III试验的数据,评价了CTH的发生率。
前瞻性观察分析了500例患者的1000次头CT结果。研究者分析了患者置管后第一次CT和最后一次CT,评价置管的精确性、CTH大小、部位和严重性。
563个导管,发现CTH 14个,首次CT和最后一次CT中21%的患者检测到CTH。大部分(86%)CTH发生在置管24h内,位于距离颅骨1cm内,至少一个直径>5mm。大部分导管(71%)尖端放置于置管部位同侧的三脑室或侧脑室。与CTH相关的因素为入院前使用抗血小板药物、导管放置的精度、手术室外放置导管、亚洲人种和脑室出血扩大。
最终作者认为导管置入之初和稳定期CTH发生率相对较低,尽管为高风险患者的紧急置管。导管放置的精确性类似于或优于以前的报道。留意放置导管的精度和手术室置管能够降低CTH的风险。抗血小板药物是CTH的独立危险因素。
原始出处:Müller A1, Mould WA1, Freeman WD2, et al. The Incidence of Catheter Tract Hemorrhage and Catheter Placement Accuracy in the CLEAR III Trial. Neurocrit Care. 2018 Aug;29(1):23-32.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ROC#
26
值得借鉴的临床经验,非常不错的学习资料,涨见识,获益匪浅,感谢分享!
60
非常不错的学习资料,值得借鉴的临床经验,学习了,获益匪浅,感谢分享!
0
#脑室外引流#
47
#脑室#
40
学习了
52