肠息肉是指一类从黏膜表面突出到肠腔内的隆起状病变,在没有确定病理性质前统称为息肉。肠息肉分布于结肠和直肠的各个部位,有单发性息肉,多发性息肉和息肉病之分,病理显微镜下分成炎性或增生性息肉、管状腺瘤、管状绒毛腺瘤、绒毛状腺瘤等类型。
对绝大部分人来说,肠息肉不会有啥特别的感觉,最多出现便血、腹泻、 腹痛等无特异性的临床表现。然而,只有当息肉变大时,可能会出现拉黑便 、便血以及经常性腹痛等较为明显的症状。
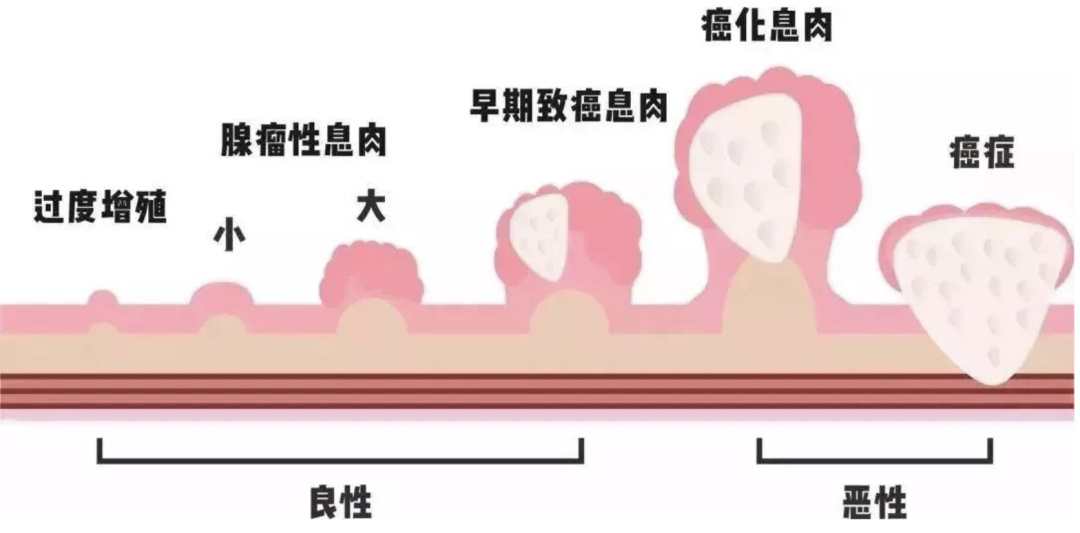
然而,肠息肉确实会癌变,且绝大多数的大肠癌都是由肠息肉恶变而来的,但不是所有的息肉都会癌变。息肉发生癌变受很多因素的影响,包括息肉的大小、类型、形态、数目、部位、上皮间变程度等等。
现已明确,息肉切除术可有效中断腺瘤至腺癌进展从而降低结直肠癌发展的风险。肠镜是息肉最主要的检出手段。在肠镜发现息肉后,光靠看是无法肯定这些息肉是非肿瘤性还是肿瘤性的,需要切下来进行病理检查,才能最终确认。最后,根据肠镜检查息肉的数目、部位、大小、形态、病理检查结果决定是否需要切除息肉。
随着内镜技术的发展,已经使得切除息肉成为非常简单,安全,有效的微创操作。多数息肉可以在内镜下切除,对于切除较困难的息肉还需不断改进切除技术以及所需的相关器械。 下面我们就来了解一下,常规结直肠息肉切除术。
一、微/小息肉切除术
常规的肠镜检查中发现,约90%的结直肠息肉为微小息肉 ( ≤ 5mm) 或小息肉 (6 ~ 9mm ),对此类息肉进行切除可有效阻断息肉癌变的进程。目前,结直肠微小息肉切除的主要方式有活检钳息肉钳夹术、圈套器息肉勒除术和氩离子凝固术。
1、活检钳息肉钳夹术
活检钳息肉钳夹术适用于直径<0.5cm的息肉,是最常用且简单的息肉切除方法。活检钳息肉钳夹术包括了冷活检钳夹术(CFP)和热活检钳夹术(HFP)。

A 钳除前,B 钳除后创面。
C-D:热活检钳除术注意事项,息肉体积过大,增加电凝时间,造成透壁性损伤
(图片来源:胃肠病)
CFP能避免与电凝有关的风险以及几乎可忽略的肠穿孔风险。最新欧洲胃肠镜学会(ESGE)指南指出,对于采用圈套器较难切除的息肉也可以选用较易操作的 CFP。
而HFP则常用于止血,因为该技术可在钳咬病灶的同时电凝其周围的部分正常组织并可术中止血,故可一定程度上提高息肉的完整切除率。然而,因HFP造成迟发型出血、穿孔等并发症发生率较高,且较难获得良好的生物组织标本用于病理学评估,所以用于结直肠息肉的内镜治疗需要谨慎。
2、圈套器息肉勒除术
圈套器息肉勒除术包括冷圈套息肉切除术(CSP)和热圈套息肉切除术(HSP),其中,HSP是目前国内结直肠微小息肉和小息肉最常用的切除方式之一,即发现小息肉后,通过活检孔道送入热圈套器后完整套取息肉,逐渐收紧圈套器后将高频发生器连接圈套器,以混合电凝切法将息肉切除。
而CSP是易于操作的技术,适用于适用于巴黎分型:0-Ip、0-Is、0-Isp 及 0-IIa。CSP圈套器是一个自包含型金属环, 有利于息肉完整切除,且不需电凝, 从而避免电凝相关并发症 。
3、氩离子凝固术
氩离子凝固术(APC)适用于治疗细小的扁平或广基息肉。APC通过特殊装置将氩气离子化后导电使其能量流向病灶组织故而凝固并灼除息肉 ,具有高效 、快速 、操作视野大 、连续凝固创面、凝固深度自限性、 创伤小、有效止血且患者耐受性好等众多优点。在消化道息肉切除术后的止血 ,以及病变灼烧中发挥着重要作用。
然而,因为息肉采用氩离子灼除,故存在难以获取病理组织标本以及了解病变的浸润深度和切缘情况等缺陷。
除以上常见术式,还有尼龙圈套扎法、金属夹结扎术、微波凝除法、热电极治疗法、激光灼烧法等等, 但对此类息肉采取何种方式切除尚无统一标准。
二、巨/大息肉切除术
对巨/大息肉来说,常用的有内镜下黏膜切除术(EMR)和内镜黏膜下剥离术(ESD)。
1、内镜下黏膜切除术
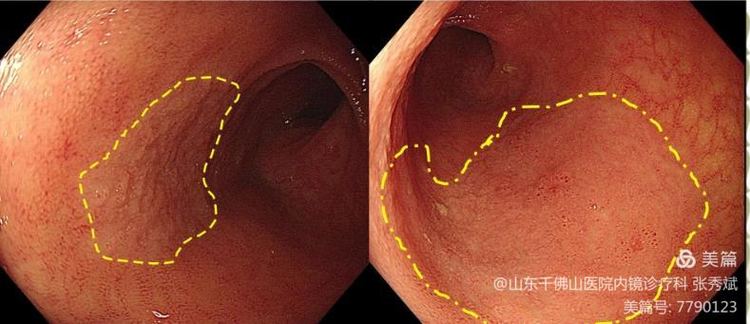
内镜下黏膜切除术(EMR)
EMR主要适用于黏膜下注射和切除,包括整块切除和分次切除,适用于<20mm的扁平息肉。EMR分为三种:透明帽法切除术、黏膜注射下切除术、黏膜注射法分片切除术。其中,黏膜注射法分片切除术与黏膜注射下切除术在操作流程上并无太大差别,只是前者病灶较大不能一次圈套切除,需要分次切除。
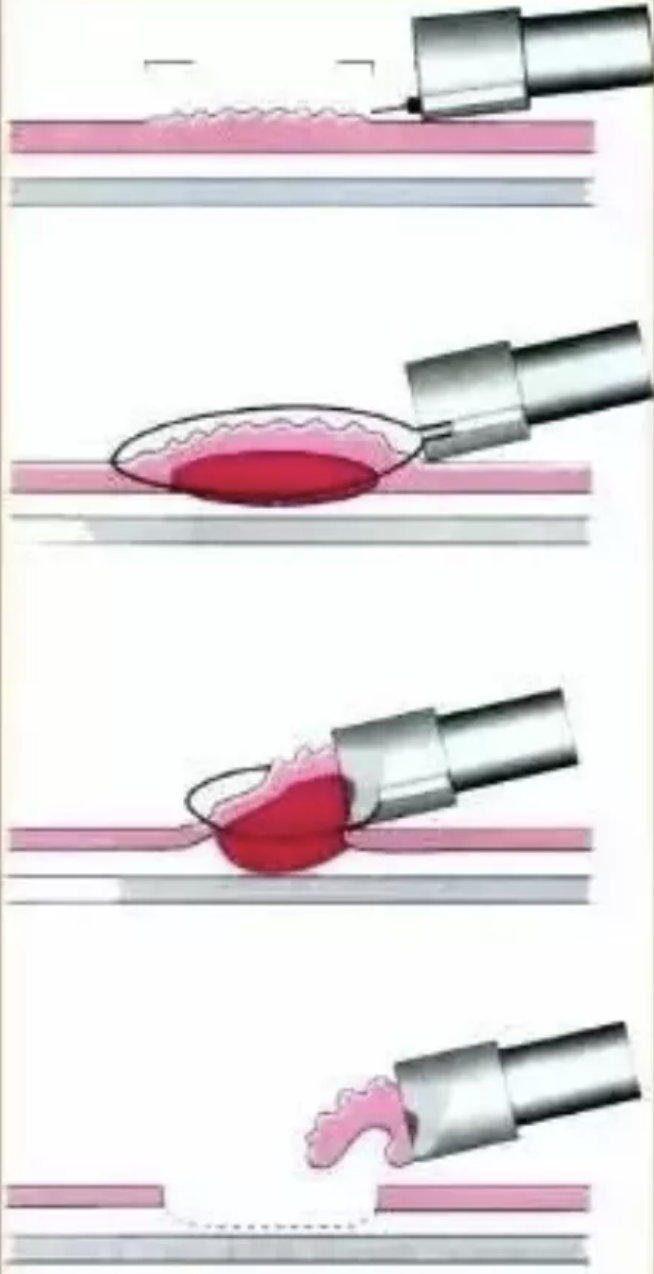
透明帽法切除术(图片来源:胃肠病)
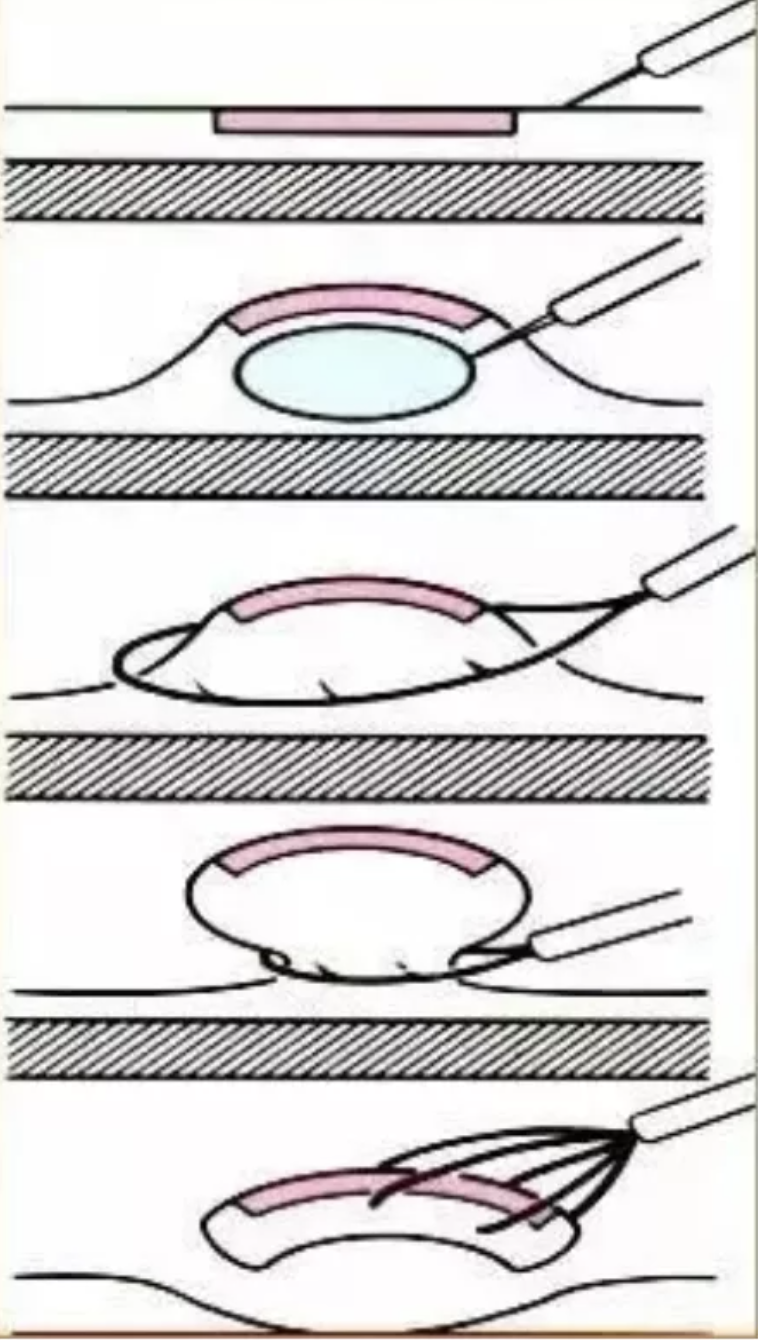
黏膜下注射切除术(图片来源:胃肠病)

黏膜注射法分片切除术(图片来源:胃肠病)
直径>20mm 的病变操作基本同上述,区别在于需用圈套器对较大病变进行分次切除,进而完整切除病变。对于绝大部分结直肠病变可通过 EMR 整块或分次切除,只有3%~10%的患者需要进一步手术。
2、内镜黏膜下剥离术
内镜黏膜下剥离术(ESD)主要适用于直径>20mm 的、无颗粒型 LST 、pit t-pat tern V 分 型 、高度不典型增生、可疑浅表黏膜浸润或其他内镜技术无法有效完整切除的病变。
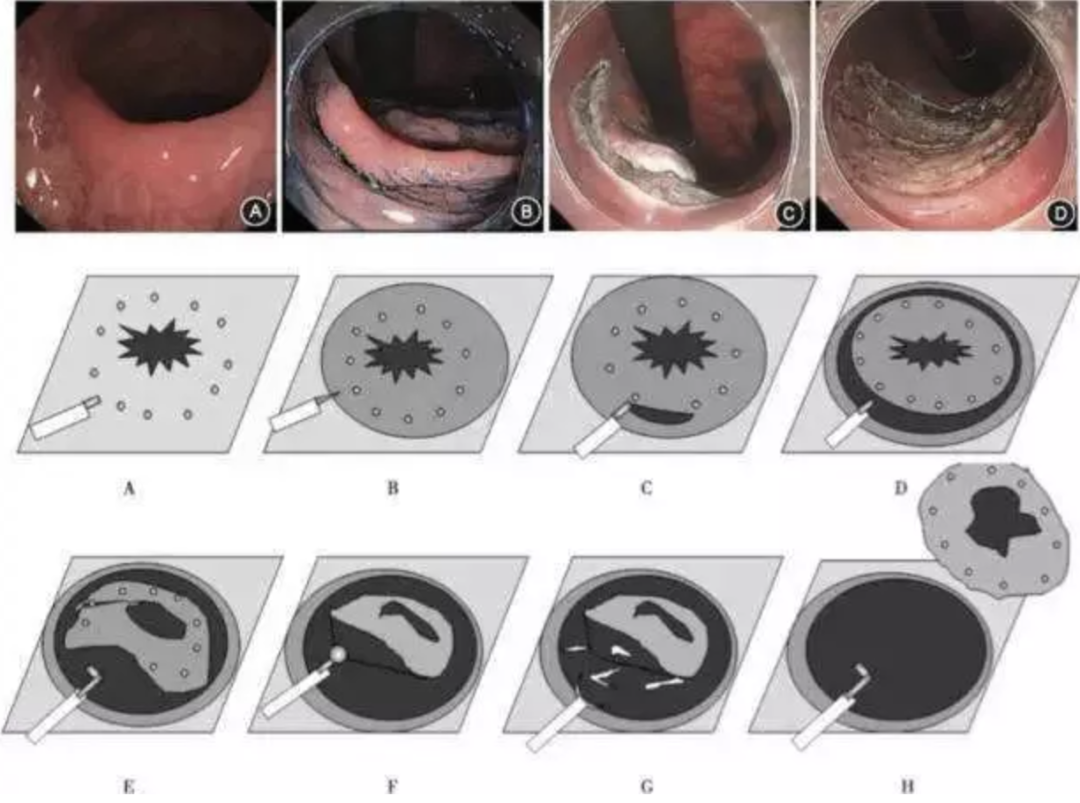
ESD图示(图片来源:胃肠病)
指南推荐:必须内镜下一次性切除的病变、部分早期癌、抬举征阴性的腺瘤、>10mm 的 EMR 后残留、复发再次行 EMR 困难的及反复活检未证实为癌的低位直肠病变亦可采用 ESD 治疗。
综上,内镜下结直肠息肉切除术是一种持续发展的内镜下治疗方法,在降低结直肠癌风险方面取得了显著的进展与成效。 胃肠病学专家需了解更多与息肉切除术有关的技术和工具,并用于内镜手术治疗中。
参考资料
1.谢娇, 王雯. 结肠镜息肉切除术及其相关技术[J]. 临床消化病杂志, 2019, 31(4):5.
2.李倩倩, 王军, 赵越,等. 结直肠息肉发生相关危险因素的研究现状[J]. 医学综述, 2020, 26(16):5.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#不同类型#
51
#切除术#
44
详细
57
#内镜下切除#
57
#内镜#
58