Ann Rheum Dis:急性焦磷酸钙晶体关节炎患者的心血管事件风险
2022-05-30 MedSci原创 MedSci原创
急性CPP晶体关节炎与非致死性CV事件的短期和长期风险升高显著相关。
已有研究表明焦磷酸钙沉积(CPPD)疾病与心血管事件(CV)风险增加相关。近日,风湿病领域顶级期刊Annals of the Rheumatic Diseases上发表了一篇研究文章,研究人员旨在调查急性焦磷酸钙(CPP)晶体性关节炎患者的CV事件风险以及CPPD的急性表现。
在1991-2017年期间,研究人员使用美国马萨诸塞州布里格姆公共医院电子健康档案(EHR)进行了队列研究。急性CPP晶体关节炎患者使用一种已发表的机器学习算法,阳性预测值为81%。

该研究的主要不良心血管事件(MACE)包括非致死性心血管事件(心肌梗死、急性冠状动脉综合征、冠状动脉重建、卒中)和死亡。研究人员估计了MACE、非致死性CV事件和死亡的发病率(IRs)和调整后的风险比,且允许在0-2年和2-10年间进行了差异估计。敏感性分析包括:(1)门诊诊断的急性CPP晶体关节炎患者,(2)2007-2016年期间伴有相关医疗保险数据的患者,(3)CV危险因素数量匹配的患者。
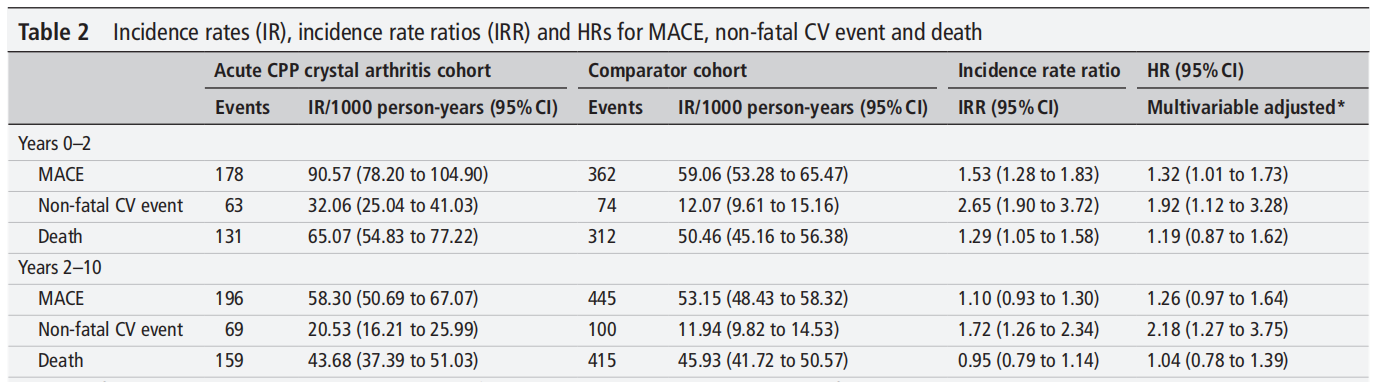
研究人员将1200名急性CPP晶体关节炎患者与3810名对照者进行了匹配。急性CPP晶体关节炎患者0-2年MACE的IR为91人/1000人/年(p-y),对照组为59人/1000人/年(p-y)。在2-10年,急性CPP晶体关节炎MACE的IR为58人/1000p-y,比较组为53人/1000p-y。急性CPP晶体关节炎与0-2年MACE(风险比为1.32,95%CI为1.01-1.73)和0-2年(风险比为1.92,95%CI为1.12-3.28)和2-10年(风险比为2.18,95%CI为1.27-3.75)非致死性CV事件风险增加显著相关,但与死亡无关。敏感性分析结果与初次分析结果相似;在门诊分析中,非致死性CVE的风险在2-10年显著升高,但在0-2年没有明显升高。
由此可见,急性CPP晶体关节炎与非致死性CV事件的短期和长期风险升高显著相关。
原始出处:
Sara K Tedeschi,et al.Risk of cardiovascular events in patients having had acute calcium pyrophosphate crystal arthritis.Ann Rheum Dis.2022.https://pubmed.ncbi.nlm.nih.gov/35613842/
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#焦磷酸钙晶体关节炎#
48
#Dis#
41
#血管事件#
48
#关节炎#
45
#心血管事件风险#
48