2022年4月,国际医学顶级期刊之一柳叶刀杂志(Lancet,IF=79.321)在线刊登了由西日本肿瘤学组和日本临床肿瘤学组(West Japan Oncology Group and Japan Clinical Oncology Group)开展完成的一项大型多中心随机对照研究JCOG0802/WJOG4607L(以下简称0802)的最终结果。
《柳叶刀》同期配发的评述“When less is more in thoracic surgery”对该结果的评价是“remarkable”。作为日本学者探索早期NSCLC最佳手术方式的研究“三部曲”之一,不同于JCOG0804和JCOG1211,0802重点研究周围型放射学侵袭性腺癌,针对该类型腺癌不同切除范围的选择可能会给患者的远期预后带来深刻的影响,而这正是近10年来0802备受瞩目的关键所在。
从2021年5月JCOG研究主席,现任世界国际肺癌研究联盟肺癌分期委员会主任浅村尚生教授(Hisao Asamura)在美国胸外科协会年会上第一次介绍0802的研究结果至今已有将近一年,现在我们终于可以直接、详尽、系统地学习体会这项关于肺段切除对比肺叶切除的经典研究。
相比于先前公布的预印本文章,最终版本延续了结论中对肺段切除适应证的表述——肺段切除术应该作为小周围型非小细胞肺癌的标准术式,但进一步充实了研究设计细节和方案施行情况,并且在per-protocal分析的基础上,补充了对主要终点的as-treated分析。
在最终版本发布的这个重要节点,再次研读回味0802研究精彩的设计、非凡的结果以及研究者不偏不倚的讨论,十分有意义。
1、JCOG关于早期肺癌手术方式的系列研究以及CTR的定义
由于之前的JCOG0804研究已经实性成分占比(CTR)<=0.25,总直径<=2cm的肺结节完全可以采用楔形切除。那么0802则更进一步,旨在评估CTR>0.5,并且<=2cm的周围型小肺癌是否也可以使用肺段切除来替代标准的肺叶切除,采用非劣效性设计。主要终点为5年总生存率(OS),次要终点为无复发生存率(RFS)、6个月和12个月的肺功能、局部复发率、术后并发症等其他一些外科手术相关指标。

主要终点达到了阳性结果,肺段切除组和肺叶切除组相比,5年OS率更高,为94.3%对91.1%(p<0.001)。
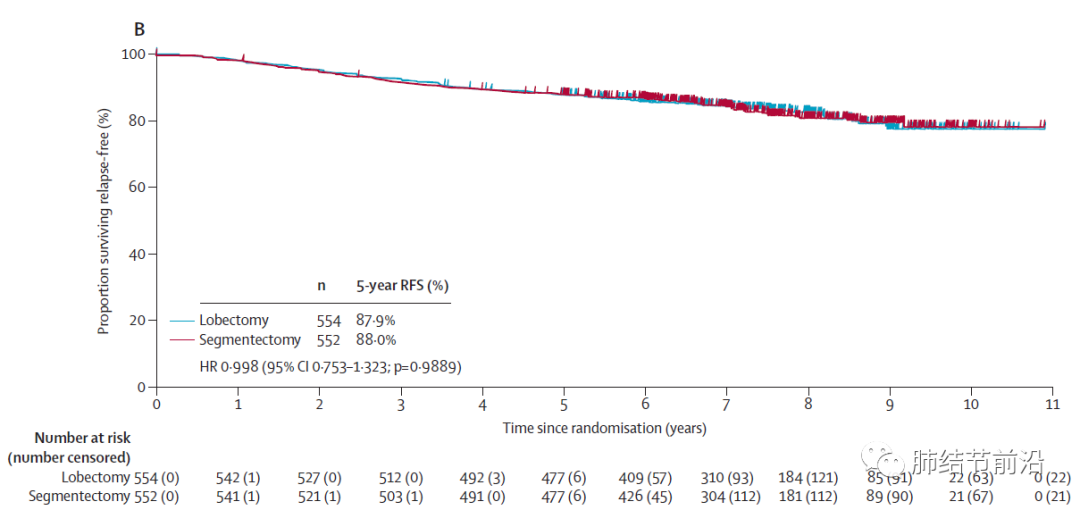
而次要终点5年RFS方面,两组几乎完全一致,肺段切除组为88.0%,肺叶切除组为87.9%。两组均有12%左右的患者5年内出现复发。
此外,术后1年肺功能方面,肺段切除后术后肺功能情况比肺叶切除肺功能提高3.5%,肺功能优势不高,没有达到预计的10%的提高。
局部复发方面,肺段切除组更高,为10.5%,而肺叶切除组为5.4%。肺段切除组局部复发概率增加约1倍。
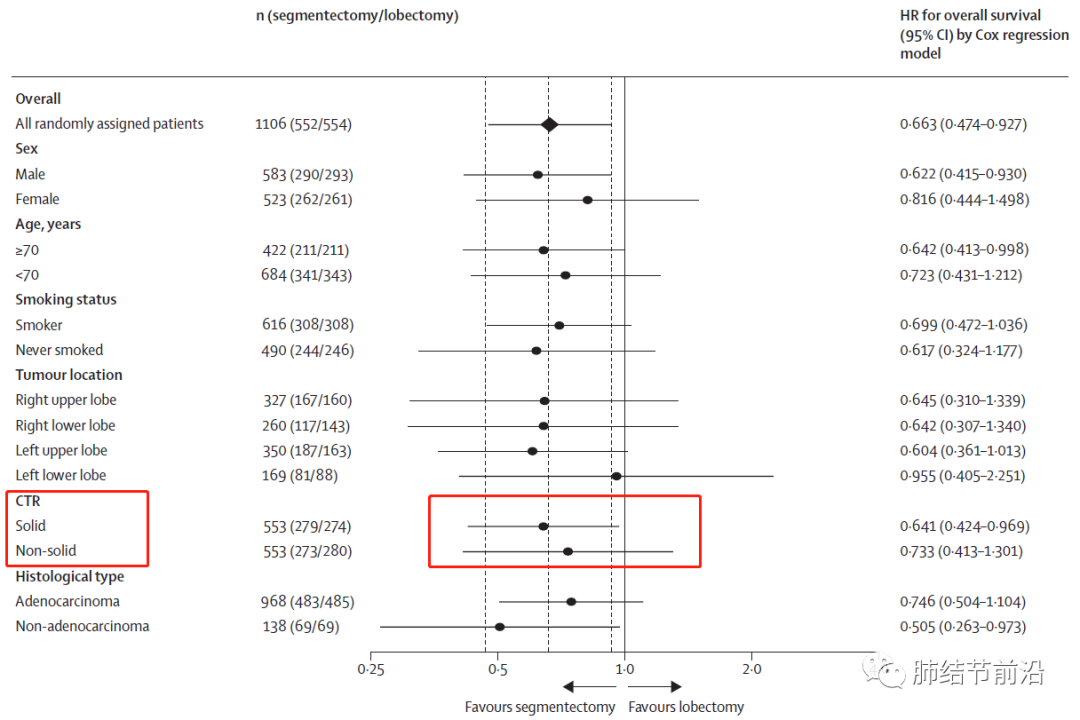
亚组分析方面,几乎全部亚组均指向肺段切除的OS更佳。包括CTR=1的纯实性结节,仍然是肺段切除的OS高于肺叶切除。
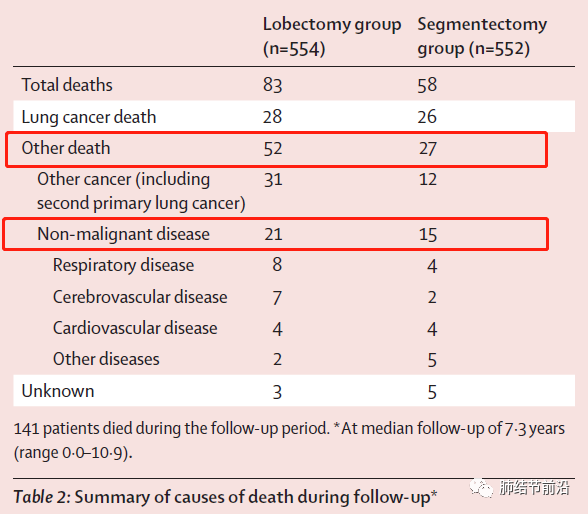
此外,肺叶切除亚组后续随访中,由于非肺癌死亡的概率似乎有所增加。包括第二原发肺癌,呼吸系统和脑血管疾病。
0802的最终结论为:由于OS达到了非劣效性的阳性结果,尽管肺段切除的肺功能保护不及预期,肺段切除仍应成为CTR>0.5,总直径<=2cm的周围型肺癌的标准手术方式。
除此之外,0802也有一些其他有用的信息:对于CTR>0.5,并且<=2cm的周围型小肺癌,肺门淋巴结转移(N1)和纵膈淋巴结转移(N2)的概率很低,约为3%。远处转移的概率更低,1106位患者中仅有1位出现了远处转移(IV期)。

2、0802凭什么可以将肺段切除术作为一种标准术式?
在研究设计伊始,JCOG团队围绕总生存和术后呼吸功能设想了四种可能的结局。浅村教授拿日本柔道来举例,一旦有选手在场上获得“一本”(一种得分形式),即获得该比赛的胜利,“一本”就相当于研究的优效性设计。但0802采取了另外一种设计,指在没有获得“一本”的情况下,获得两个“技有”等于取得了“一本”,也就是说,如果肺段切除的肿瘤学疗效非劣,且6个月或12个月时FEV1相对于肺叶组的差值超过了10%,相当于取得了两个“技有”,也是“一本”,我们就可以认为肺段切除术优于肺叶切除术。
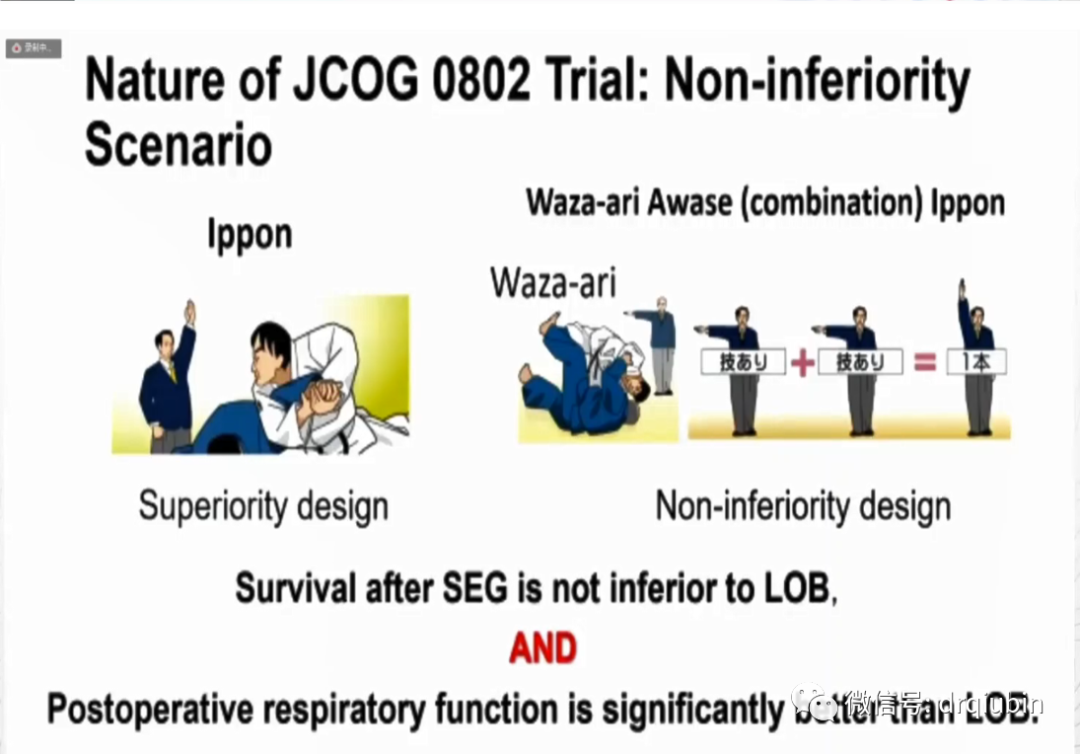
而肺段切除最终出乎绝大多数人的意料,在一项非劣效研究中取得了主要终点的优效性,取得了“一本”,直接胜出。换成大家更熟悉的足球来说,相当于欧冠决赛,教练和球迷希望自己的队伍在客场0:0逼平对手,下一场取得主场优势后1:0小胜,总比分1:0获得最终的胜利,但0802就偏偏讲述了一个客场主场都获胜的夺冠故事。
3、0802带来了哪些重要启发?
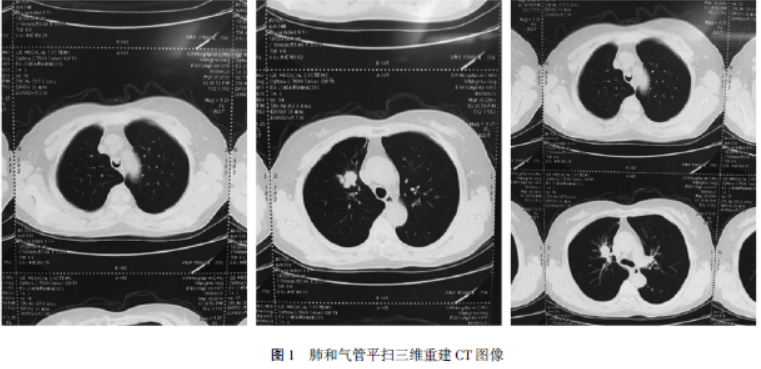
首先在局部复发上,肺段组的复发率差不多是肺叶的两倍,但并没有对OS带来显著的影响。这个结果,值得我们反复慎重地思考。肺段切除的切缘控制目前可以通过术前三维重建的规划进一步完善,那么,淋巴结清扫呢?
0802没有给出段间淋巴结的数据,但是随访中出现淋巴结转移的患者占局部复发中很大的一部分,说明淋巴结清扫的策略也要再加以定夺。2cm以内的肺结节,有相当一部分可以不做系统彻底的清扫,这样节省时间,也符合微创理念,但也不能过于乐观。术中淋巴结的冰冻病理,有些情况是必要的。同时,因为肺段组针对复发进行了积极的再治疗,带来了OS的实际获益,体现了对早期肺癌进行全程的个体化管理的价值。
然后是亚组分析结果,纯实性肿瘤在肺段组的结果很惊喜。纯实性结节往往比部分实性结节的分化情况更差,不少医生倾向于只在GGO中进行亚肺叶切除,0802的结果有助于肺段切除术的适应证在实性结节中的扩大。但话说回来,出现局部复发的,有多少是实性结节?如果绝大多数是实性结节,GGO几乎不复发,那是否说明亚肺叶切除的适应证可以朝更大尺寸的GGO扩展?JCOG1211的初步结果表明,对于3cm以内,CTR<0.5的GGO,肺段切除的5年RFS和5年OS都达到了98%以上。那么,会不会对3cm以内的周围型肺结节,只要含有GGO成分,不是纯实性,肺段切除都可以作为标准手术方案呢?
在本文的最后,笔者提供了JCOG0802这篇文章的期刊原文以及中文翻译,欢迎各位同道参考、收藏、转发!
关注肿瘤新前沿公众号,回复“0802”即可获得!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#JCO#
47
#亚肺叶#
33
#Lancet#
28
#肺叶切除#
49
学习了#学习#
53
lancet上果然牛,感谢梅斯更新及时
29