JACC:心肌自噬越活跃,扩张型心肌病患者预后越好!
2022-03-07 Nebula MedSci原创
发生左心室逆向重构的扩张型心肌病患者发生心血管事件的风险较低
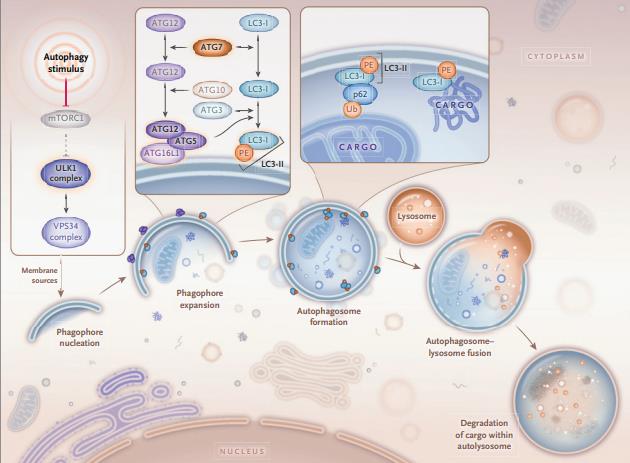
自噬是一种正常的细胞过程,其降解细胞自身的细胞质成分以提供能量并维持适当的细胞内环境。左心室逆向重构 (LVRR) 有望为扩张型心肌病 (DCM) 患者提供更好的预后。
本研究旨在评估自噬在左心室逆向重构中的作用,以及自噬在人类衰竭心脏中的预后意义。
研究人员收集了42位DCM患者(21位LVRR阳性和21位LVRR阴性)和7位正常心功能对照患者的左心室内膜心肌活检样本,予以光学显微镜下一般形态测量、免疫组织化学和免疫荧光标记分析LC3和组织蛋白酶D以及电子显微镜观察。
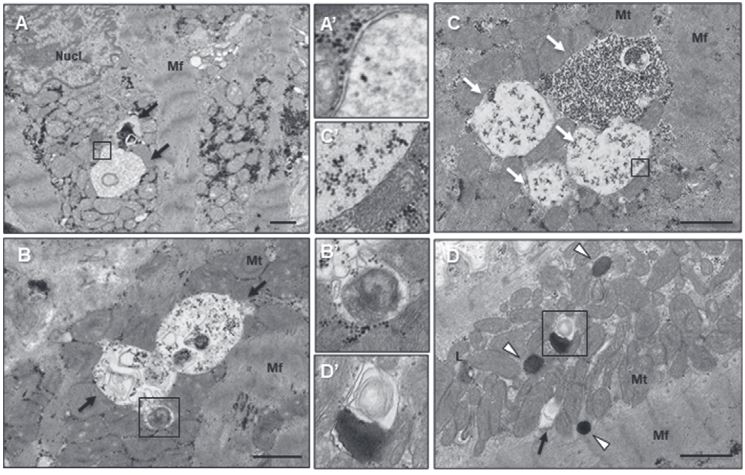
心肌细胞的电子显微镜观察
左心室逆向重构阳性患者的临床特征与左心室逆向重构阴性患者的临床特征相似,但肺动脉压和左心房大小有所差异。无论有无存在左心室逆向重构,DCM患者标本的光学显微镜下形态测量没有明显差异。电子显微镜显示,与对照个体的心肌细胞相比,在DCM患者的心肌细胞中,自噬泡(自噬体和自溶酶体)和溶酶体明显富集。
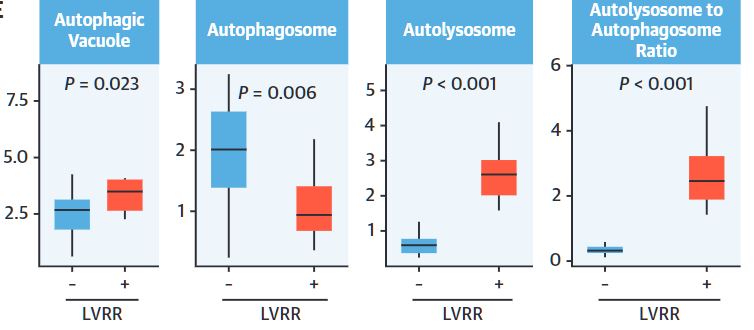
有无左心室逆向重构的心肌细胞的自噬泡、溶酶体数量
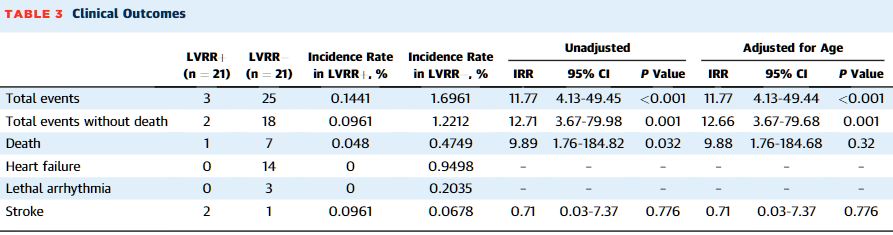
此外,与来自左心室逆向重构阴性患者的心肌细胞相比,来自左心室逆向重构阳性患者的心肌细胞含有明显更多的自噬泡,具有更高的自溶酶体比率和组织蛋白酶D表达水平。根据年龄调整的逻辑回归分析表明,自噬泡数量和组织蛋白酶D表达的升高可预测左心室逆向重构的存在与否。最后,发生左心室逆向重构的DCM患者在随访期间心血管事件的发生率较低。
有无左心室逆向重构患者的临床预后
综上,该研究表明自噬是预测DCM患者有无发生左心室逆向重构的有用标志物。该研究为治疗衰竭的DCM心脏的策略提供了新的病理学见解。
原始出处:
Kanamori Hiromitsu,Yoshida Akihiro,Naruse Genki et al. Impact of Autophagy on Prognosis of Patients With Dilated Cardiomyopathy.[J] .J Am Coll Cardiol, 2022, 79: 789-801. https://doi.org/10.1016/j.jacc.2021.11.059.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#扩张#
56
#JACC#
38
#患者预后#
31
学习了
54
学习一下
56
学习了,受教
58
学以致用!
59
学习
0
学习
25
#ACC#
31