JCO:化疗加上原发性肿瘤切除并不能提升晚期结直肠癌患者的疗效
2021-02-10 MedSci原创 MedSci原创
鉴于PTR继之化疗未显示比单纯化疗无生存获益,因此PTR不再应被视为无症状原发性肿瘤和同步性不可切除转移的CRC患者的治疗标准。
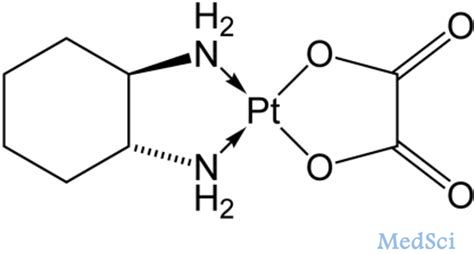
鉴于PTR继之化疗未显示比单纯化疗无生存获益,因此PTR不再应被视为无症状原发性肿瘤和同步性不可切除转移的CRC患者的治疗标准。 对于无法治愈的晚期大肠癌(CRC)患者,初始治疗策略仍存在争议。因此该研究评估了对标准化疗增加无创原发肿瘤切除术(PTR)对无症状原发性肿瘤和最多3个不可切除转移灶的不可切除IV期CRC患者的生存获益。2月9日,Journal of Clinical Oncology发布文章,报告了这项III期随机对照研究的结果(JCOG1007,iPACS研究; UMIN标识符:UMIN000008147)。iPACS是第一个研究PTR在转移性CRC癌症患者中的作用的RCT。 在2012年6月至2019年9月之间,该研究共纳入165名患者入选,并使其随机分配为单独接受化疗(84例)或PTR+化疗。该研究调查了在无法切除的IV期无症状CRC和仅限于肝、肺和远处淋巴结转移的三种或以下不可切除的转移性疾病患者中,PTR联合化疗与单纯化疗相比在总生存(OS)方面的优势。 165例患者中有120例(73%)最常见的不可切除的转移性疾病是肝转移。两组不可切除的转移性疾病的分布相似。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#原发性#
41
#肿瘤切除#
53
#JCO#
38
#晚期结直肠癌#
40
感谢各位
72
学习了
67
不错不错
57
#结直肠#
35
#原发性肿瘤#
44
晚期
81