CGH: 生物制剂时代到来后炎症性肠病患者肠道切除和结肠切除术的发生率变化
2022-04-18 xuyihan MedSci原创
生物制剂为一种比较新的、效果较为理想的抗风湿药,是近二十多年来风湿免疫领域较大的进展之一,目前应用于类风湿关节炎 、脊柱关节炎、系统性红斑狼疮等的治疗。
炎症性肠病 (IBD) 的治疗目标包括实现临床和内镜缓解、预防疾病进展以及减少手术干预等。在IBD中,手术的终生风险在克罗恩病 (CD) 中为50%至80%,在溃疡性结肠炎 (UC) 中约为30%。在过去的 20 年中,生物单克隆抗体的引入彻底改变了 IBD 的医学方法,据报道,CD 患者的使用率高达 40%,UC 患者的使用率高达 16%。生物制剂可以实现黏膜愈合,这与中度至重度 IBD 患者的临床反应和缓解有关。这种愈合是否会改变 IBD 的自然史存在争议。多项研究表明,生物制剂可能会降低 CD 的肠道切除率和 UC 的结肠切除率;然而,也有一些研究得出了相互矛盾的结果。因此,本项研究旨在探究接受和不接受生物制剂治疗的 IBD 患者的肠切除和结肠切除术的患病率。
研究人员使用了包括来自美国 26 个主要综合医疗保健系统的电子健康记录数据进行了数据采集。将所有在 2015 年至 2020 年期间接受过任何生物制剂治疗的 CD 或 UC 患者纳入本项研究。主要观察结果是检查生物制剂治疗与肠切除患病率之间的关联。此外,研究人员还确定了与 IBD 患者使用生物制剂进行手术相关的因素。

在数据库中的 32904480 名患者中,研究人员确定了 140540 名 CD 患者和 115260 名 UC 患者,其中分别有 25840 名(18%)和 9050 名(7.8%)患者接受了生物制剂治疗。与未接受生物制剂治疗的患者 (12.1%) 相比,接受生物制剂治疗的 CD 患者 (9.3%) 的肠切除率显着降低 (p<.001)。同样,与未接受生物治疗的 UC 患者 (11.0%) 相比,接受生物治疗的 UC 患者接受结肠切除术的可能性显着降低 (7.3%) (p<.001)。抽烟、艰难梭菌感染和肛周疾病与 CD 的肠道切除有关。结肠肿瘤和艰难梭菌感染与 UC 的结肠切除术有关。
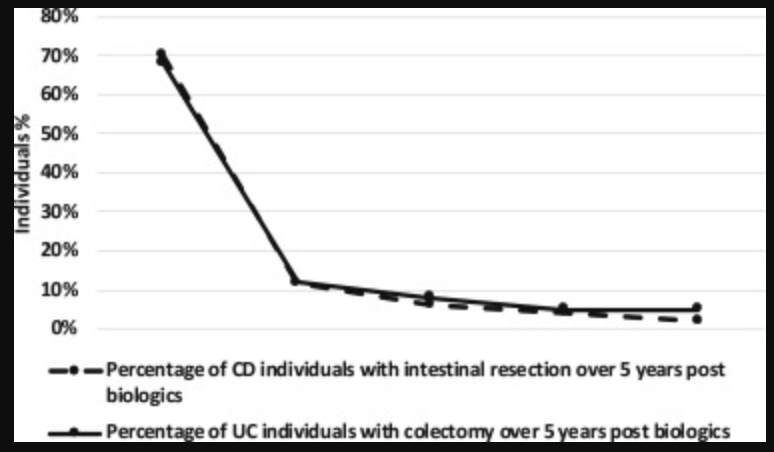
在这项针对大型医疗保健管理数据库的研究中,研究人员发现与从未接受过生物制剂的患者相比,接受过生物制剂治疗的炎症性肠病 (IBD) 患者进行肠切除的可能性显着降低。该数据表明,生物制剂可能会影响 IBD 的手术率。
原始出处:
George Khoudari. Et al. Rates of Intestinal Resection and Colectomy in Inflammatory Bowel Disease Patients After Initiation of Biologics: A Cohort Study. Clinical Gastroenterology and Hepatology. 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#CGH#
37
#结肠切除术#
38
#生物制剂#
62
#发生率#
38
#切除术#
36
#炎症性#
36
#炎症性肠病患者#
34