新研究显示,英国青年人中非酒精性脂肪肝的发病率高达20%
2019-04-15 不详 MedSci原创
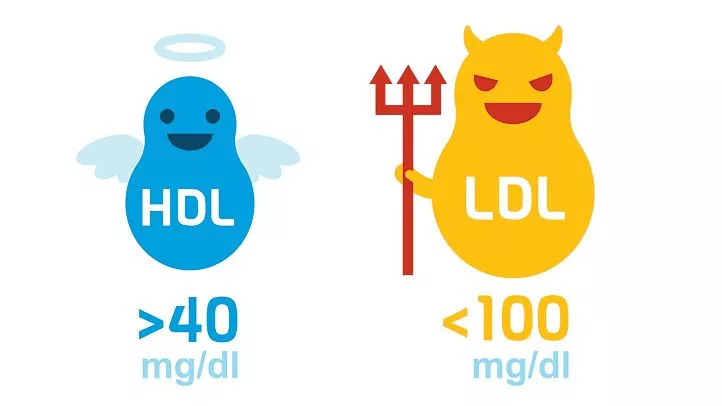
新的研究显示,英国年轻人中非酒精性脂肪性肝病(NAFLD)患病率奇高,其中40%已经进展为纤维化。该研究内容由布里斯托尔大学在2019年奥地利维也纳举行的国际肝病大会上发布。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#发病率#
28
#酒精性脂肪肝#
27
#青年人#
33
#酒精性#
35
#非酒精性#
32