Science:华人科学家发现HIV新位点 推动疫苗进展
2016-05-14 张蔚然 中国新闻网
原题:美国科学家取得艾滋病毒研究重要进展 美国国家卫生研究院当地时间12日宣布,该院科学家针对艾滋病毒的研究取得重要进展,在艾滋病毒上发现了一个新的位点,该发现为艾滋疫苗的探索和研究打开了一条新的路径。 这一研究成果已于12日在美国《科学》杂志在线发表,论文的第一作者是美国国家卫生研究院过敏与传染病研究所下属疫苗研究中心的3位华人科学家,分别是孔瑞、许凯和周同庆,他们的研究方向包括抗体和疫苗
美国国家卫生研究院当地时间12日宣布,该院科学家针对艾滋病毒的研究取得重要进展,在艾滋病毒上发现了一个新的位点,该发现为艾滋疫苗的探索和研究打开了一条新的路径。
这一研究成果已于12日在美国《科学》杂志在线发表,论文的第一作者是美国国家卫生研究院过敏与传染病研究所下属疫苗研究中心的3位华人科学家,分别是孔瑞、许凯和周同庆,他们的研究方向包括抗体和疫苗、蛋白质结构和疫苗。
该研究院在声明中说,艾滋疫苗研究的策略之一是通过免疫方法诱导出能有效针对重要靶点的中和抗体,然而由于艾滋病毒的多变性,这样的靶点很有限。该院科学家们在艾滋病毒上发现了一个新的位点,这个位点可以被免疫系统产生的抗体分子识别,从而可以作为疫苗研究的新靶点,科学家也发现了这种抗体的作用机制。鉴于此,该发现为艾滋疫苗的探索和研究打开了一条新的路径。
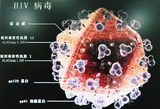
据介绍,这项研究发现的新靶点在艾滋病毒膜蛋白上,由一段连续的8个氨基酸组成,是艾滋病毒融合肽的一部分。在此之前,艾滋病毒的融合肽没有被科学家视为疫苗设计的靶点。所以,此项发现的主要意义在于挖掘出艾滋病毒的一个“软肋”。以往的艾滋疫苗设计主要针对一些结构非常复杂的位点,设计难度很大,而融合肽的结构要简单很多,针对融合肽的疫苗设计有可能相对容易。
卫生研究院说,基于此项最新发现,该院科学家正集中精力设计新型疫苗,试图诱导出类似的融合肽抗体。
原始出处:
Kong R, Xu K, Zhou T, Acharya P, Lemmin T, Liu K, Ozorowski G, Soto C, Taft JD, Bailer RT, Cale EM, Chen L, Choi CW, Chuang GY, Doria-Rose NA, Druz A, Georgiev IS, Gorman J, Huang J, Joyce MG, Louder MK, Ma X, McKee K, O'Dell S, Pancera M, Yang Y, Blanchard SC, Mothes W, Burton DR, Koff WC, Connors M, Ward AB, Kwong PD, Mascola JR. Fusion peptide of HIV-1 as a site of vulnerability to neutralizing antibody. Science. 2016 May 13;352(6287):828-33. doi: 10.1126/science.aae0474.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#科学家发现#
37
#新位点#
0
#SCIE#
25
#华人#
29
厉害啊
169
厉害啊
114
华人籍科学家 不是中国
95
最近来看,艾滋病的疫苗,研究进展非常迅速,有可能就在最近几年有,关键性突破,未来艾滋病不再是难题了。
131
最近来看,艾滋病的疫苗,研究进展非常迅速,有可能就在最近几年有,关键性突破,未来艾滋病不再是难题了。
117