Circulation:心衰患者贫血与缺铁,现有概念与新兴疗法
2018-07-23 石岩 环球医学
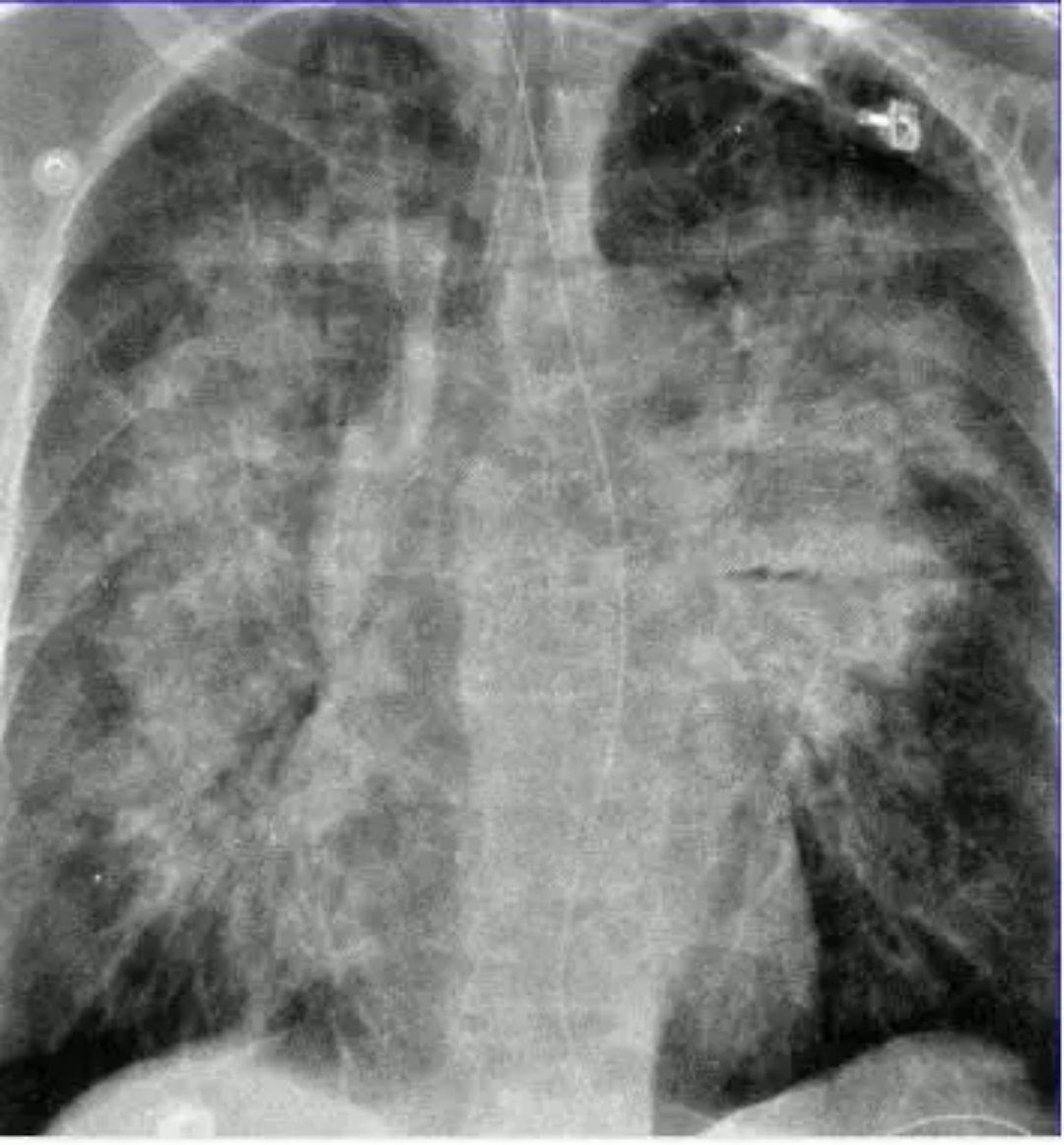
贫血和缺铁是重要且常见的合并症,在心衰患者中常常同时存在。这两种症状同时或单独存在均与较差的临床状态和更差的结局相关。贫血和缺铁只是心衰严重度的指标?它们是否影响心衰进展和结局并因此需要进行治疗?目前仍不清楚。2018年7月,发表在《Circulation》的一项由美国学者进行的综述,探讨了心衰患者贫血与缺铁的原因和治疗方案的选择。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












全面综述
60
借鉴大家经验很棒
59
跟大家学习很好
68
学习一下很不错
50
#心衰患者#
34
#缺铁#
31