JACC-Clinical Electrophysiology:房颤内外科混合(Hybrid)消融的有效性和安全性
2022-01-09 “Clinic門诊新视野”公众号 “Clinic門诊新视野”公众号
近些年来,新型口服抗凝药物(NOACs)、导管消融、左心耳封堵(LAAC)等药物与器械治疗方式的兴起与发展为非瓣膜性房颤患者预防脑卒中提供了很好的帮助,房颤相关的致残率、致死率显著下降。
近些年来,新型口服抗凝药物(NOACs)、导管消融、左心耳封堵(LAAC)等药物与器械治疗方式的兴起与发展为非瓣膜性房颤患者预防脑卒中提供了很好的帮助,房颤相关的致残率、致死率显着下降。然而,对于非阵发性、且难治性的房颤患者而言,当前的治疗结局依旧不尽如人意;针对这类人群,临床上不仅也在积极探索各种联合治疗措施,如:“胸腔镜下消融+导管消融”的混合(Hybrid)消融术式,但这类治疗方式的有效性与安全性尚未完全明确。2021年12月,Pavel Osmancik等人于JACC:Clinical Electrophysiology上发布了一项小样本的单中心、单臂、前瞻性临床试验,对上述问题予以了初步解答。

研究背景与目标
尽管针对房颤的筛查诊疗技术进展飞速,但非阵发性心房颤动(AF)患者当前的治疗结局仍未达到令人满意的状态。经典的Cox迷宫手术虽是积极有效的治疗选择,但并不适用于一般的AF人群。在过去十年间,AF的手术治疗已逐渐从外科转为微创手术。而为了确保在胸腔镜下完整识别病变、并成功消融那些外科医师难以处理的结构,临床上提出了“胸腔镜下消融+导管消融”的混合(Hybrid)消融术式,并已成功将之用于非阵发性房颤患者的临床治疗之中。
不过,相较于导管消融,胸腔镜下消融似乎有着更高的并发症风险,包括:卒中;据悉,当前尚无研究证实可以完全解决胸腔镜消融期间的无症状卒中以及后续的认知功能下降问题。基于这样的消融现状,研究人员特别发起和开展了这项单中心、单臂、前瞻性试验,旨在借助连续ILR心电图(ECG)记录、脑磁共振成像(bMRI)和认知功能检查等高敏感度方法来评估混合消融的有效性和安全性。
试验设计以及主要终点
这一前瞻性观察研究纳入的均为有症状、药物难治性、非阵发性AF患者。入组前,所有患者均接受了心脏病学检查,包括:超声心动图、CTCA(或单纯冠状动脉造影)、肺活量测定和胸部X光检查。根据研究设计,非阵发性AF患者会在非体外循环状态下,接受使用COBRA Fusion射频系统(Estech)的胸腔镜下消融术以完成环肺静脉(PV)隔离,并同期使用AtriClip Pro行左心耳(LAA)封堵。外科消融术后2-3个月,研究人员会进行分期电生理(staged EP)评估和导管消融(CA)治疗。所有患者均在出院前植入ILR(Reveal LinQ)以评估窦性心律(sinus rhythm,SR)维持情况,并在EP研究完成后第30天、90天、180天、270天和360天时进行随访,而后再每个6月到院随访评估一次。
研究的主要有效性终点(SR OFF Survival)为无心律失常生存(arrhythmia-free survival),即:停用抗心律失常药物、重做消融或心脏复律后无房颤或房性心动过速发作;次要有效性终点(SR ON Survival)为AT或AF再次发生,需要重启AAD、复律或再消融,但在实施上述抗心律失常措施后没有进一步发作AF或AT。
主要安全性终点方面,所有患者在外科消融住院期和出院前都会进行标准临床检查,死亡、卒中或短暂脑缺血发作、转为胸骨切开术、需要重新探查的出血以及其它严重影响住院时长或致残的不良事件均被认为是主要并发症。此外,患者还会在基线时(术前1天)、术后(2-4天行脑磁共振成像或术后1月行神经心理学检查)和远期(EP术后6月或胸腔镜消融术后9月)时行脑功能磁共振成像(bMRI)和神经心理学检查。
结果与讨论
自2017年5月至2019年6月,该研究总计纳入59名符合入排标准的非持续性房颤患者(年龄:62.5±10.5岁),其中37名(62.7%)为男性,平均随访时间为30.3±10.8个月;共55(93.2%)例患者成功进行了胸腔镜消融术,其中54例患者(91.5%)成功完成LAA封堵,仅1名患者因特别年轻(24岁)而特意未作封堵。
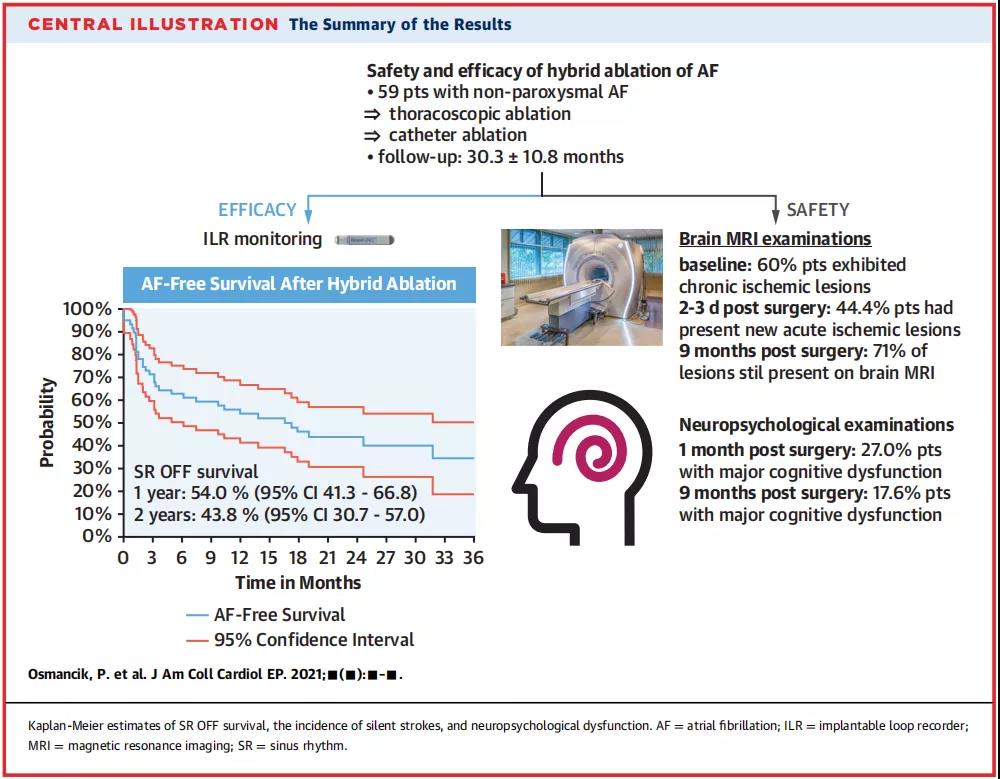
图1. 中心图说
从bMRI检查结构来看,60.0%的患者基线时存在慢性缺血性脑损伤;44.4%的患者术后2-4天时的磁共振成像提示出现新发缺血性病变;术后9月时,71%的缺血性病变依然存在(图1)。
神经心理学检查则提示,术后1月和9月时,分别有27.0%和17.6%的患者存在严重的术后认知功能障碍(POCS)。另外,随访1年的无心律失常生存率为54.0%(95% CI:41.3-66.8);随访2年的无心律失常生存率为43.8%(95% CI:30.7-57.0)(表1)。
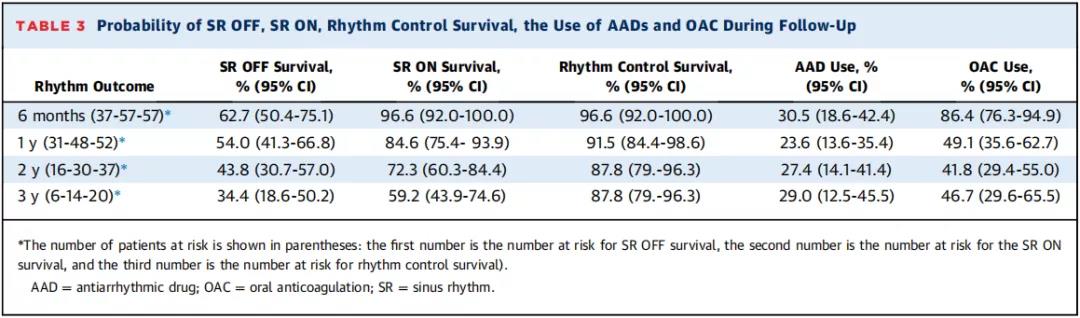
表1. 随访期内SR OFF/SR ON存活率、节律控制存活率、AAD/OAC使用率
针对上述随访结果,研究人员指出,尽管胸腔镜下消融是在心外膜上进行,但消融环上绝大部分被消融的病变是透壁的,术前桥接LWMH、术前和术后立即减少抗凝、心脏复律后心房顿抑和全身麻醉等都可能导致血栓前状态的增加。目前,很难判断胸腔镜下消融可能带来的不利影响能否为恢复窦性心律提供的积极影响所抵消,大量无症状脑损伤病例的存在无疑是对临床的一种警告。
另外,从神经心理学评估结果来看,入组患者在胸腔镜下消融术后1月和9月的POCD发生率分别为27.0%和17.6%,这种早期较高的POCD患病率可能反应了麻醉的可逆效应,而晚期的认知障碍比例则可能反映了术中的直接脑损伤问题。
总 结
总体而言,该项小样本研究反映了胸腔镜下消融与无症状脑缺血的高风险相关,内外科Hybrid消融的中期疗效一般。不过,由于该研究并未设置导管消融对照组,故并不能完全呈现消融过程中无症状脑缺血事件的风险差异。未来,这一问题有待进一步探索和明确。
原始出处:
Pavel Osmancik, et al. The Efficacy and Safety of Hybrid Ablations for Atrial Fibrillation. JACC: Clinical Electrophysiology, Volume 7, Issue 12, December 2021, Pages 1530-1532.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
0
#Physio#
39
已学习
50
#ACC#
40
#消融#
32
#clinical#
24