Hypertension:十秒心率变异性越高,高血压风险越低,年轻人尤其!
2022-03-28 MedSci原创 MedSci原创
较高的心率变异及其在10秒心电图上随时间的增加与较低的高血压风险有关。
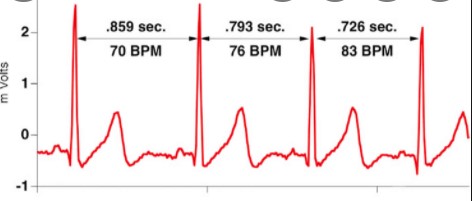
心率变异性(HRV)是指逐次心动周期之间细微的时间变化及其规律,是评价自主神经系统的交感-副交感神经张力及其平衡的重要指标。HRV对于疾病的预后判断有着重要价值,可应用于心源性和非心源性疾病的危险分层,HRV降低是预测心脏病患者死亡的危险因子。
健康的心脏拥有健康的“不规律”,HRV测的就是心跳的不规律性。心跳的不规律性是由自主神经主导的;因此,HRV能够反映神经系统的健康。通常来说HRV越高越好。高HRV代表更好的心血管功能和抗压能力,而低HRV意味着更高的焦虑抑郁风险,以及更高的心血管疾病的死亡率。
目前有关HRV的作用及其在发生高血压时的时间变化尚不清楚。为了研究10秒心率变异性及其变化与年龄小于40岁的成年人的高血压事件之间的关系,来自韩国的学者开展了相关研究,结果发表在Hypertension杂志上。
这项队列研究包括232 587名没有高血压的韩国人(平均年龄37.6岁)。高血压是根据2017年美国心脏病学院和美国心脏协会高血压指南定义的。心率变异,包括连续RR间期差异的均方根和正常至正常RR间期的SD,是用标准的12导联10秒心电图估计的。
在3.8年的中位随访期间,发现了40268个高血压病例(年轻人和老年人的发病率分别为每36.1和67.9/1000人年)。总的来说。心率变异和高血压风险之间观察到了一种剂量依赖性的反向关系,即变异性越高,高血压风险越低。
比较连续RR间隔差异的均方根和正常-正常RR间隔的SD,高血压的多变量调整危险比(95%CI)分别为1.58(1.52-1.63)和1.35(1.30-1.39)。这些关联在青壮年中比在老年人中更强。在150个301人的子样本中,与稳定的心率变异相比,心率变异随着时间的推移而增加也与发生的高血压呈反比关系。
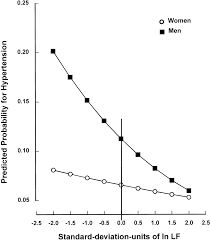
较高的心率变异及其在10秒心电图上随时间的增加与较低的高血压风险有关。用10秒标准心电图估计的自律神经功能在预测高血压方面起着作用,对年轻成年人的影响更大。
参考文献:
Ten-Second Heart Rate Variability, Its Changes Over Time, and the Development of Hypertension. Hypertension. 2022;0:HYPERTENSIONAHA.121.18589
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#PE#
45
#TENS#
32
#变异#
35
#心率变异性#
55
#Hypertension#
44