Gastric Cancer:符合扩大适应症标准的早期胃癌内镜黏膜下剥离技术难度的相关因素
2020-07-02 MedSci原创 MedSci原创
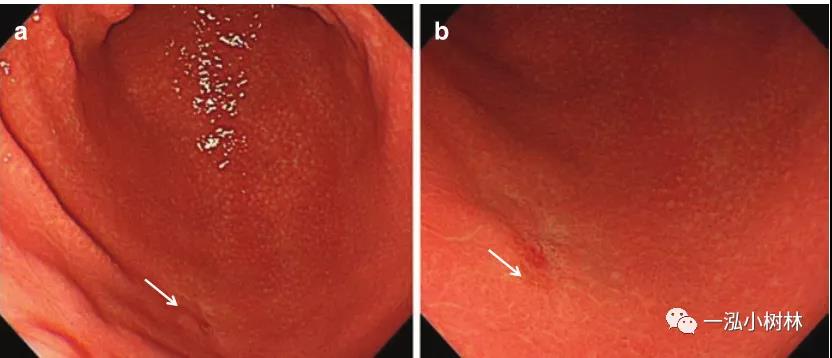
关于胃内镜黏膜下剥离术(ESD)的技术难度的报道很少。本研究旨在利用ESD扩大适应症标准的多中心非随机确诊试验(JCOG0607)数据,探讨早期胃癌(EGC)ESD技术难度的相关因素。
关于胃内镜黏膜下剥离术(ESD)的技术难度的报道很少。本研究旨在利用ESD扩大适应症标准的多中心非随机确诊试验(JCOG0607)数据,探讨早期胃癌(EGC)ESD技术难度的相关因素。
主要纳入标准如下:(1)组织学证明的肠型腺癌;(2)cT1aN0M0;(3)病变未发现溃疡(UL-阴性),大小>2cm,或UL阳性,≤3cm;(4)年龄20-75岁。疑难病例定义为ESD耗时≥120 min,片状切除,和/或手术过程中出现穿孔。
结果,2007年6月至2010年10月,共有来自29家机构的470例患者入组。中位手术时间为79(范围14-462)min,127例患者手术时间≥120min。12例患者在ESD过程中出现穿孔,其中9例患者手术时间≥120 min。因此,130例(27.7%)患者被确定为疑难病例。多变量分析显示,>5 cm的UL阴性(vs≤3 cm的UL阴性,几率比,24.993;95% CI 6.130-101.897,p<0.0001)几率比最大,其次是胃上部或中部3-5 cm的UL阴性,年龄≤60岁与难度显著相关。
综上所述,该结果表明,UL阴性病灶大于3 cm、胃的上段或中段、年龄≤60岁是与EGC的ESD技术难度相关的独立因素。
原始出处:
Tomonori Yano, Noriaki Hasuike, et al., Factors Associated With Technical Difficulty of Endoscopic Submucosal Dissection for Early Gastric Cancer That Met the Expanded Indication Criteria: Post Hoc Analysis of a Multi-Institutional Prospective Confirmatory Trial (JCOG0607). Gastric Cancer. 2020 Jan;23(1):168-174. doi: 10.1007/s10120-019-00991-3.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#gastric#
35
#GAS#
24
#AST#
33
#内镜#
35
#适应症#
27
#相关因素#
33
#黏膜#
34
ESD难度报道
97