Case Rep in Pulmono:原发性肺癌隐匿发展,低钠血症患者的非小细胞癌与小细胞癌并存
2019-02-03 李胜佳 医博士
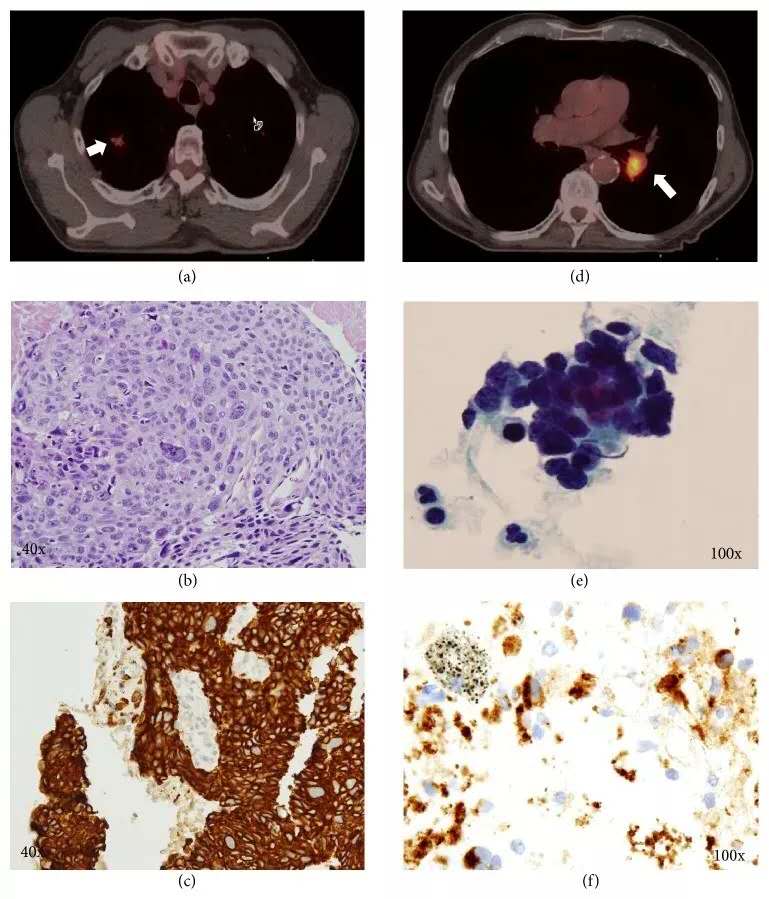
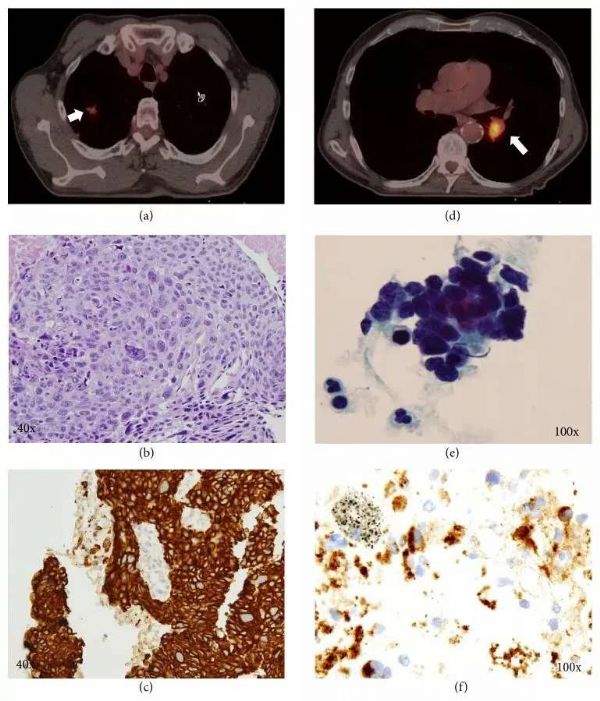
患者男性,66岁,有50年的吸烟史和严重的慢性阻塞性肺疾病(COPD),计算机断层扫描(CT)复查结果显示右上叶新发(RUL)肺结节和左下叶(LLL)慢性实变。患者肺功能检查(PFTS)显示气流阻塞,FEV1为2.58 L(81%预测)。6个月前的胸片上LLL实变明显,当地的肺科医生通过常规支气管镜活检检查该病灶,未发现恶性肿瘤的证据。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
33
#case#
37
#非小细胞#
40
#原发性#
36
#小细胞癌#
49
#隐匿发展#
23
#低钠血症#
32
#低钠#
24
#原发性肺癌#
36
#隐匿#
33