European Urology:根治性前列腺癌切除术后局部复发的抢救性手术可行性
2021-03-18 MedSci原创 MedSci原创
PSMA-PET阳性患者精囊床内局部复发的抢救性手术是可行的。它可能为选择性的局部复发患者提供了延长无BCR生存期和增加TFS的机会。

pixabay.com
在前列腺癌(PCa)中,即使是在以治疗为目的的初级治疗(如根治性前列腺切除术(RP))之后,也经常观察到复发。由于前列腺特异性膜抗原(PSMA)正电子发射断层扫描(PET)成像的引入,即使在非常低的前列腺特异性抗原(PSA)水平下,RP术后后孤立的局部复发可以被准确地描绘出来。
据报道,在0-0.19、0.2-0.49、0.5-0.99、1-1.99和≥2 ng/ml的PSA范围内,检测率分别为33%、45%、59%、75%和95%。这种评估复发的无创方法为更准确地应用局部治疗创造了机会。因此,建议生化复发(BCR)患者在作出治疗决定之前进行PSMA PET显像。(前列腺癌生化复发是指前列腺癌根治手术,或根治性放疗达到根治效果后,如果PSA连续两次超过0.2ng/mL,但影像学上未发现复发或转移病灶,提示前列腺癌生化复发。)
为了描述和评估前列腺癌术后精囊床局部复发患者抢救性手术的手术技术、生化反应和无治疗生存(TFS)。有研究者回顾性评估了两个中心(2014年11月-2020年2月)40例接受开放式抢救手术的患者。所有患者均表现为RP后生化复发(BCR),PSMA PET显像表现为单一局部复发。33例(82.5%)曾接受过挽救性放射治疗。该研究结果近日发表在European Urology杂志上。
评估6-16周后前列腺特异性抗原(PSA)最低点和未经进一步治疗(PSA<0.2ng/ml)的完全生化反应(cBR)患者百分比。采用Kaplan-Meier估计法计算无BCR生存率和TFS。对Clavien-Dindo并发症进行评估。
研究结果显示,抢救性手术前,PSA中位数为0.9 ng/ml(四分位间距[IQR]:0.5 1.7 ng/ml)。术后PSA最低点中位数为0.1ng/ml(IQR:0.4ng/ml)。在31例(77.5%)患者中观察到cBR(完全生化反应率,定义为PSA<0.2ng/ml)。在平均24.4个月的随访中,22例(55.0%)患者出现BCR,12例(30.0%)患者接受进一步治疗。随访1年,无BCR生存率62.2%,TFS生存率88.3%。观察到3例(7.5%)Clavien-DindoⅢ级并发症。主要局限性是回顾性设计,随访时间短,缺乏对照组。
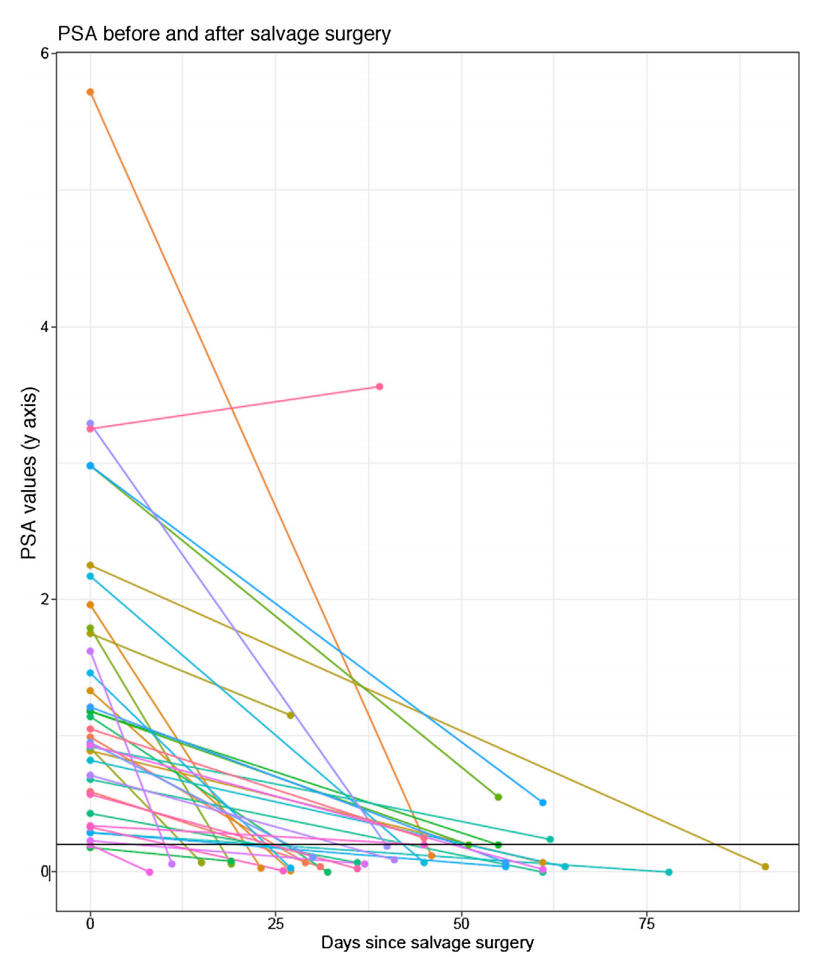
2014年11月至2020年2月,在两个中心接受抢救性手术的37例患者的PSA在抢救性手术后3个月内下降
当考虑挽救性手术时,复发病灶的准确定位是很重要的,由于直肠或括约肌损伤的风险太高,功能结果(尤其是节制)可能受损,因此不应通过手术接近吻合口区域的病变。此外,术中对复发组织的可靠识别往往具有挑战性。它可能很小,形态难以辨认,或隐藏在纤维化组织中。在这里,PSMA-RGS的术中指导非常有价值。PSMA-RGS在抢救过程中提供了进一步的安全性,因为它用于术中测量,以促进复发病灶的定位。此外,在挽救性淋巴结清扫中,与传统的非引导手术方法相比,增加放射引导似乎可以提高挽救性手术的疗效。
总之,PSMA-PET阳性患者精囊床内局部复发的抢救性手术是可行的。它可能为选择性的局部复发患者提供了延长无BCR生存期和增加TFS的机会。需要进一步的研究来证实这项研究发现。
参考文献:Knipper, S., Ascalone, L., Ziegler, B., Hohenhorst, J. L., Simon, R., Berliner, C., … Maurer, T. (2020). Salvage Surgery in Patients with Local Recurrence After Radical Prostatectomy. European Urology. doi:10.1016/j.eururo.2020.11.012
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#局部复发#
49
#PE#
31
#切除术#
26
#可行性#
25
#局部#
39
#抢救#
34
#根治#
28
前列腺癌相关研究,学习了,谢谢梅斯
53