JAMA Neurol:作为取栓术的补救措施,动脉内溶栓的疗效
2020-04-30 杨中华 脑血管病及重症文献导读
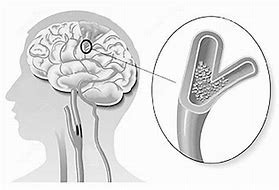
成功再灌注-理想完全再灌注(TICI 3)-是大血管闭塞性急性缺血性卒中机械性血栓切除术(mechanical thrombectomy,MT)患者功能预后的最相关和可修改的决定因素。
成功再灌注-理想完全再灌注(TICI 3)-是大血管闭塞性急性缺血性卒中机械性血栓切除术(mechanical thrombectomy,MT)患者功能预后的最相关和可修改的决定因素。然而,几乎每十名患者中就有一例患者未达到再灌注,并且根据HERMES协作组织和大型登记研究的数据,大多数成功治疗的患者并未达到TICI 3。因此,对于手术失败或旨在实现完全再灌注(TICI 3)而不是近全再灌注(TICI 2b)的情况下,MT 后寻找其他辅助治疗方法可能能够改善患者的预后。
动脉内给予溶栓剂,比如组织纤溶酶原激活物(tPA)或尿激酶原/尿激酶,选择其中之一可能时一种有希望的治疗选择。然而,作为第二代MT设备辅助治疗措施,动脉内溶栓安全性和有效性的数据很匮乏。
2020年3月来自瑞士的Johannes Kaesmacher等在 JAMA Neurology 上公布了他们的研究结果,目的在于探讨 MT 治疗失败或不完全再灌注后动脉内给予尿激酶的疗效。
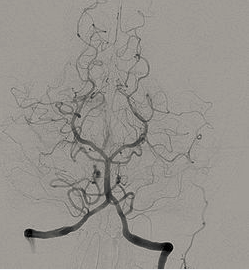
在这个回顾性队列研究中纳入了从2010年1月到2017年4月间连续的患者,这些患者经过了二代 MT 治疗,其中993例符合前循环大血管闭塞的入选标准,100例患者在 MT 失败或不全 MT 后使用手动微导管动脉内注射了尿激酶。主要安全性终点为 sICH(Prolyse in Acute Cerebral Thromboembolism II criteria),二级终点为90天死亡率和90天功能独立(mRS <=2)。按照血管造影评价有效性(TICI 分级)。
平均年龄74.6岁。使用尿激酶的最常见原因为 MT 后不全再灌注(TICI<3),占53%。调整基线特征后,动脉内尿激酶与 sICH(aOR, 0.81; 95%CI, 0.31-2.13)或90天死亡率(aOR, 0.78; 95%CI, 0.43-1.40)增加无关。在53例部分互殴近全再灌注并且动脉内使用了尿激酶的患者中,60.4%达到了早期再灌注改善,34%达到了 TICI 分级的改善。相应地,调整选择偏倚(有利于动脉内尿激酶组不良 TICI 分级)后,动脉内使用尿激酶患者的功能独立率更高(aOR, 1.93; 95%CI, 1.11-3.37)。
最终作者认为,对于经过筛选的患者,MT期间或 MT 后动脉内给予尿激酶时安全的,可以提高血管造影的再灌注。尚需要进行多中心前瞻性登记研究后随机临床试验系统性地评价这种方法。
原始出处:Johannes Kaesmacher, Sebastian Bellwald, Tomas Dobrocky, et al. Safety and Efficacy of Intra-arterial Urokinase After Failed, Unsuccessful, or Incomplete Mechanical Thrombectomy in Anterior Circulation Large-Vessel Occlusion Stroke. JAMA Neurol. 2019 Dec 9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#取栓术#
0
#动脉内溶栓#
35
#Neurol#
27
#取栓#
32
谢谢梅斯提供这么好的信息,学到很多
42
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
34