Radiology:评价AD患者脑组织铁含量水平不要再用老一套!影像学及解剖学上的新角度
2021-06-15 shaosai MedSci原创
铁是人体中普遍存在的元素,并且是主要生化过程(如氧化磷酸化,氧转运以及神经递质和DNA合成)不可缺少的辅助因子。
 铁是人体中普遍存在的元素,并且是主要生化过程(如氧化磷酸化,氧转运以及神经递质和DNA合成)不可缺少的辅助因子。据报道,在许多神经退行性疾病中均可发现铁的蓄积异常。但是,铁蓄积的增加与这些疾病的发病机制的关系尚不明确。已有研究表明,阿尔茨海默病(AD)患者较高的脑铁浓度与β-淀粉样斑块和神经纤维缠结有关。
铁是人体中普遍存在的元素,并且是主要生化过程(如氧化磷酸化,氧转运以及神经递质和DNA合成)不可缺少的辅助因子。据报道,在许多神经退行性疾病中均可发现铁的蓄积异常。但是,铁蓄积的增加与这些疾病的发病机制的关系尚不明确。已有研究表明,阿尔茨海默病(AD)患者较高的脑铁浓度与β-淀粉样斑块和神经纤维缠结有关。
现阶段,神经成像技术可在体内检测顺磁性脑组织铁含量。多项研究表明,R2*弛豫率mapping可定量评估脑组织中的铁沉积。大部分有关AD研究的已经探讨了深灰质中的铁含量,并发现AD患者基底神经节(BG)的铁含量高于健康对照组(HC)参与者。然而只有少数研究评估了BG外AD的铁沉积,这可能具有潜在的临床意义,但由于磁化率的邻近性和不连续性的影响,使用梯度回波MRI评估仍然具有挑战性。且据我们所知,目前还没有发表过关于AD患者新皮质铁含量变化与认知能力下降之间关系的研究。
近日,发表在Radiology杂志的一项研究通过使用R2*弛豫率mapping技术比较了AD患者和年龄匹配的HC患者之间脑组织整体和区域铁含量差异,并评估了AD患者在17个月随访期间的纵向R2*变化,并确定了铁含量数据与认知能力下降的关系,为临床进一步阐明AD的发生机制及病理过程提供了参考依据,为AD的早期诊断及治疗提供了技术支持。
本项前瞻性研究对2010年至2016年招募的AD患者和2010年至2014年期间招募的年龄匹配的HC患者进行了评估。在100名AD患者中,56人在平均随访17个月的时间内接受了随后的神经心理测试和脑MRI检查。所有参与者均接受了包括对宏观B0场不均匀性进行校正的R2* mapping MRI检查。对解剖结构进行分段,并计算新皮层、皮层叶、基底节(BG)、海马和丘脑的中位R2*值。采用多变量线性回归分析,研究AD组间R2*水平的差异以及R2*值的纵向变化与认知的关系。
共100名AD患者(平均年龄73±9岁[标准差];58名女性)和100名年龄匹配的HC参与者(平均年龄73±9岁;60名女性)进行了评估。AD组的BG(HC, 29.0 sec-1;AD, 30.2 sec-1,P = 0.01)、总新皮层(HC, 17.0 sec-1;AD, 17.4 sec-1;P < .001)、枕叶(HC, 19.6 sec-1;AD, 20.2 sec-1;P = .007)和颞叶(HC, 16.4 sec-1;AD, 18.1 sec-1;P < .001)的中位R2*水平均高于HC组。在AD患者中,颞叶R2 *值与阿尔茨海默病总评分的纵向变化(β = -3.23分/ sec-1,P = 0.003)有关,而与脑容量的纵向变化无关。
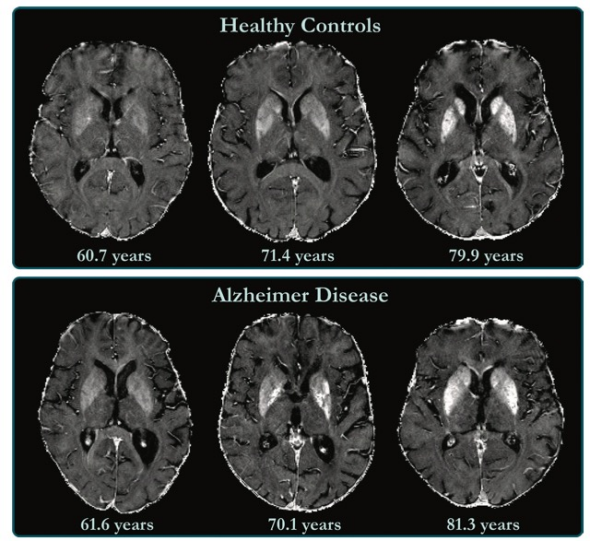
图1 健康对照参与者和AD患者的R2⁎map。基底神经节中铁浓度的差异太小,无法在AD患者和健康对照者之间通过视觉进行分别,并且铁含量水平在很大程度上取决于解剖结构和受试者年龄。
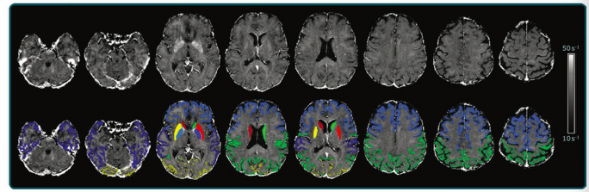
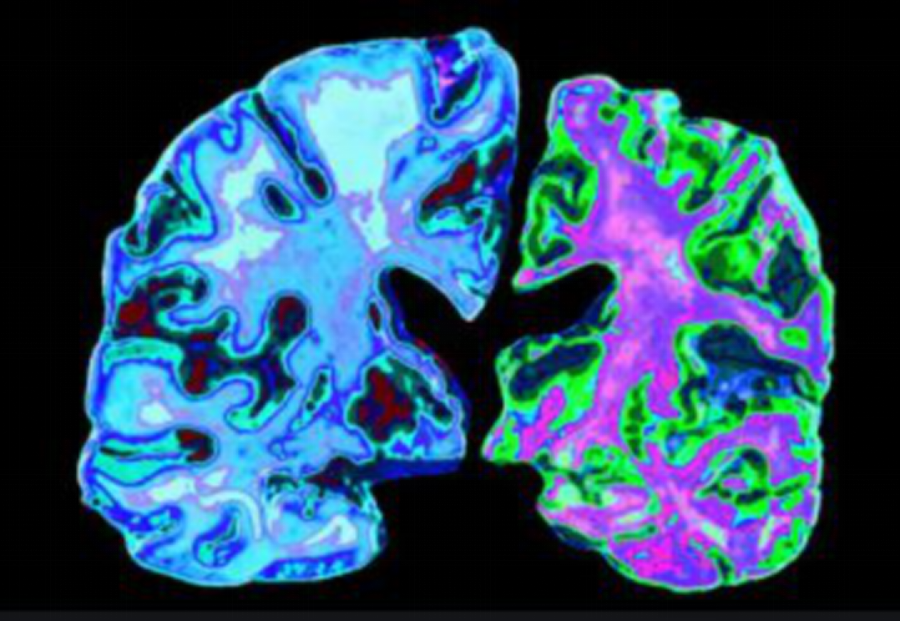
图2 研究中一位参与者的叠加了皮质和皮质下分割的R2⁎map。
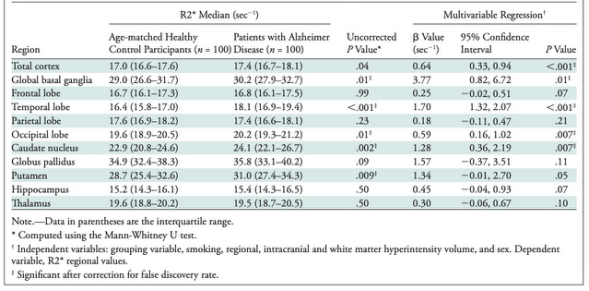
表 AD患者和健康对照组参与者不同脑区的R2 *值。
本研究表明,阿尔茨海默病患者深部灰质和新皮质区的铁含量高于健康对照组。随着时间的推移,颞叶铁含量的变化与阿尔茨海默病患者的认知能力下降有关。本研究有助于临床对阿尔茨海默病病理生理的深入理解,同时也为记你一步的相关研究提供了新的思路。
原文出处:
Anna Damulina,Lukas Pirpamer,Martin Soellradl,et al.Cross-sectional and Longitudinal Assessment of Brain Iron Level in Alzheimer Disease Using 3-T MRI.DOI:10.1148/radiol.2020192541
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#铁含量#
51
#评价#
38
#脑组织#
34
#解剖学#
39