J Clin Hypertens:沙库巴曲缬沙坦ARNI治疗亚洲人群难治性高血压结果发布
2022-03-18 MedSci原创 MedSci原创
沙库巴曲缬沙坦刚刚获批高血压适应证,之前发表的多项沙库巴曲缬沙坦高血压临床研究中已观察到其显著降压疗效。而且,沙库巴曲缬沙坦最初就是作为一种降压药来研发的。从机制上来说,除了具有缬沙坦成分抑制肾素-血
沙库巴曲缬沙坦刚刚获批高血压适应证,之前发表的多项沙库巴曲缬沙坦高血压临床研究中已观察到其显著降压疗效。而且,沙库巴曲缬沙坦最初就是作为一种降压药来研发的。从机制上来说,除了具有缬沙坦成分抑制肾素-血管紧张素-醛固酮系统(RAAS)外,其含有的沙库巴曲成分还可增强利钠肽系统,排钠排水、直接舒张血管。因此,这种集多种降压机制于一身的药物能够产生更强的降压效果。
对于难治性高血压来说,临床治疗方案中通常含有RAAS抑制剂血管紧张素转换酶抑制剂(ACEI)/血管紧张素受体拮抗剂(ARB),同时合并使用其他降压药。沙库巴曲缬沙坦本身含有缬沙坦成分,若用其替代原治疗方案中的ACEI/ARB,并在其他药物应用不变的情况下,难治性高血压患者的血压控制或许能够得到明显改善,但尚缺乏依据。
在高血压患者中,难治性高血压患病率约为10%~20%,此类人群的血压控制是临床面临的一大重要挑战。近日,由大连医科大学附属第一医院姜一农教授牵头国内7家医院开展的关于血管紧张素受体脑啡肽酶抑制剂(ARNI)在亚洲难治性高血压患者中疗效的研究发表在Journal of Clinical Hypertension,为难治性高血压治疗提供了新证据,姜一农教授和宋玮教授为共同通讯作者。
本研究包括4周筛选期和8周治疗期。筛选期对患者进行难治性高血压的筛查评估和相关检查,符合条件者进入8周治疗期。使用ARB者直接替换为200 mg沙库巴曲缬沙坦治疗,使用ACEI者应停药36小时后再替换,其他药物继续使用。如果4周后血压仍未控制,则将沙库巴曲缬沙坦剂量增至400 mg(图1)。最终66例患者完成研究,其中37例药物剂量从200 mg增至400 mg以达到降压目标。基线时,56.1%的患者使用3种降压药(包括噻嗪类利尿剂)、43.9%使用4种降压药控制血压。
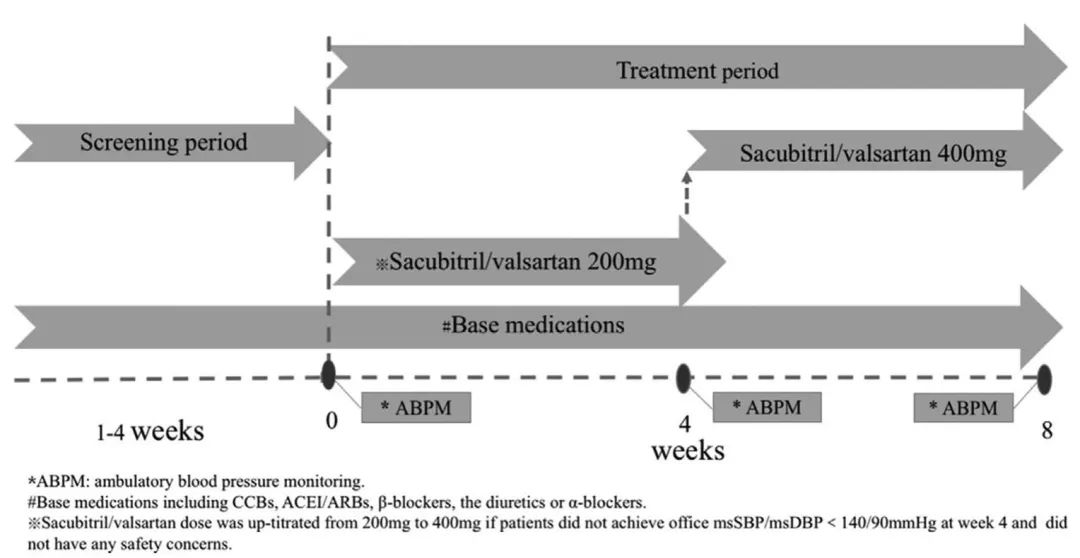
图1. 研究设计
本研究与这些研究治疗方案不同,难治性高血压患者先经过4周标准治疗,若血压未达标则将ACEI/ARB替换为沙库巴曲缬沙坦,患者应用的其他治疗不变。从研究结果来看,治疗第4周和第8周的降压效果均很明显。诊室血压在第4周时平均降低13.0/9.9 mm Hg,第8周时降幅达19.4/11.8 mm Hg(图2)。
之所以产生如此明显的降压效果,分析原因之一是研究观察人群为难治性高血压患者。中国大约60%高血压患者为盐敏感性高血压,难治性高血压人群中这一比例更高,若不限盐排钠,此类人群血压很难下降。而沙库巴曲缬沙坦可以覆盖高血压发病的多种机制,具有迅速起效的较强的利钠利水和直接扩张血管作用,多重作用产生强效降压效果。本研究中患者除了应用沙库巴曲缬沙坦,还继续使用之前应用的其他降压药如钙通道阻滞剂(CCB)、利尿剂、β受体阻滞剂(BB)等,与沙库巴曲缬沙坦的降压机制也会产生协同降压效果。这也反映出对于难治性高血压来说,利钠利水很重要,多种机制同时干预更重要。
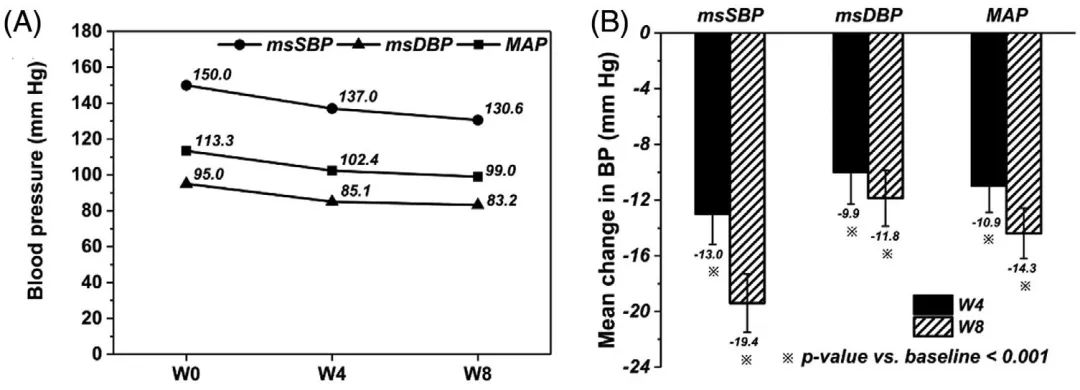
图2. 沙库巴曲缬沙坦治疗后,诊室血压和平均动脉压的(A)变化和(B)自基线的降幅
误差线代表标准误。msSBP,平均坐位收缩压;msDBP,平均坐位舒张压;MAP,平均动脉压
从本研究来看,治疗8周时平均动态收缩压下降16.6 mm Hg,日间(6:00~22:00)动态收缩压降幅17.5 mm Hg,夜间(22:00~6:00)降幅15.8 mm Hg(图3)。按比例来说,夜间血压下降更大。既往有研究比如将沙库巴曲缬沙坦与奥美沙坦进行比较,也发现夜间血压降幅差别超过日间。
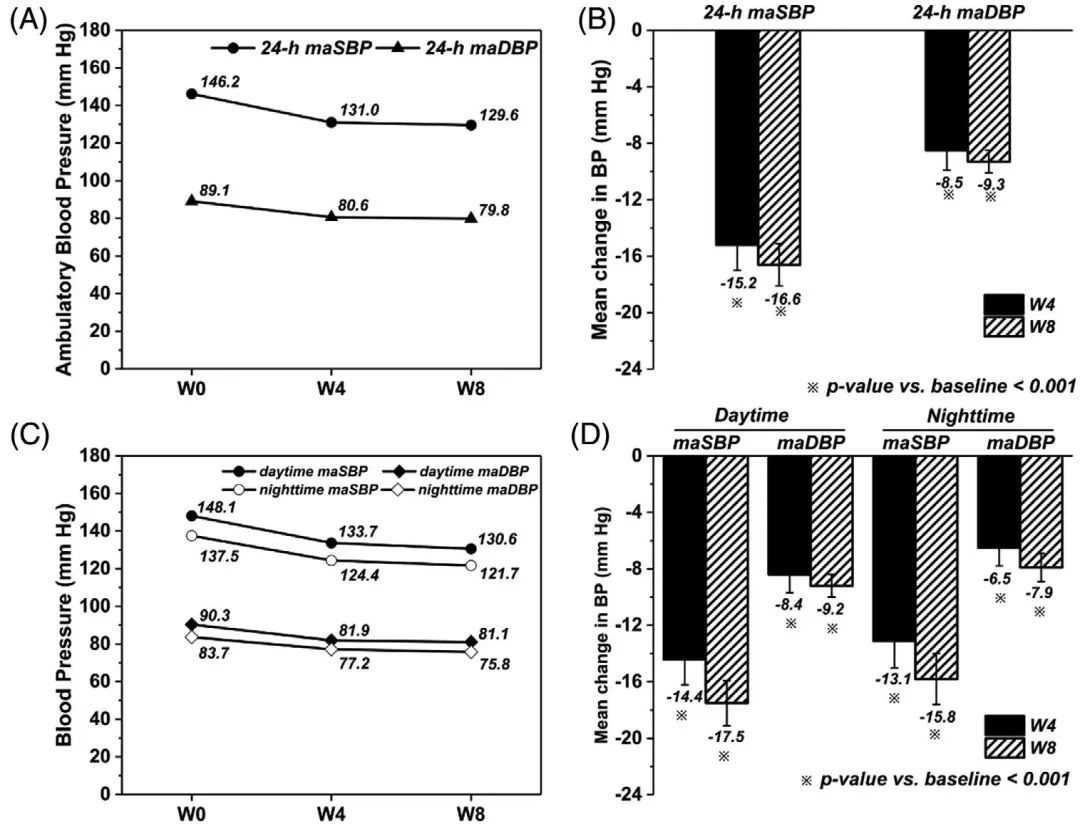
图3. 沙库巴曲缬沙坦治疗后,(A)24小时和(C)日间及夜间的maSBP和maDBP的变化、(B)24小时和(D)日间及夜间的maSBP和maDBP自基线的降幅
误差线代表标准误。maSBP,平均动态收缩压;maDBP,平均动态舒张压
在研究人群方面,难治性高血压患者大多合并代谢综合征,年龄偏大(50多岁),服用多种降压药无法使血压达标,高血压发生涉及多重机制。而沙库巴曲缬沙坦能够很好地涵盖高血压的多种发病机制,独特的利尿利钠作用使其在难治性高血压治疗中更具优势。对于亚洲高血压人群来说,盐敏感性高血压较常见,容量负荷重者较多,可能更适合应用沙库巴曲缬沙坦,相比其他人种应用的降压幅度可能更大。
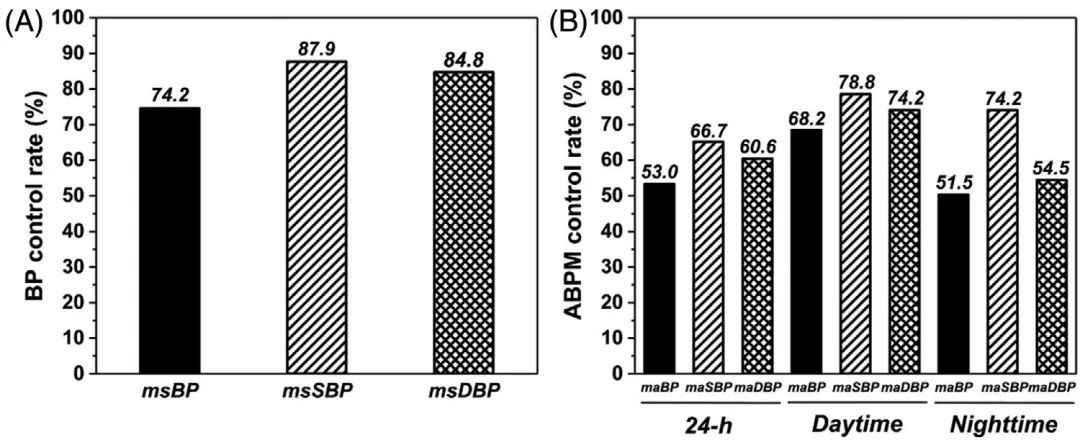
图4. 沙库巴曲缬沙坦治疗后,(A)诊室msBP(<140/90 mm Hg)、msSBP(<140 mm Hg)和msDBP(<90 mm Hg)的控制率以及(B)maBP(24h maSBP/maDBP<130/80 mm Hg、日间maSBP/maDBP<135/85 mm Hg、夜间maSBP/maDBP<120/70 mm Hg)、24h maSBP(<130 mm Hg)、24h maDBP(<80 mm Hg)、日间maSBP(<135 mm Hg)、日间maDBP(< 85 mm Hg)、夜间maSBP(<120 mm Hg)和夜间maDBP(<70 mm Hg)的控制率
msBP,平均坐位血压;msSBP,平均坐位收缩压;msDBP,平均坐位舒张压;maBP,平均动态血压;maSBP,平均动态收缩压;maDBP,平均动态舒张压
研究表明,在难治性高血压患者的 8 周治疗期间,沙库巴曲/缬沙坦可使诊室血压降低 19.4/11.8 mmHg。该试验的结果与日本一项研究中沙库巴曲/缬沙坦的降压效果一致。他们发现慢性肾病 (CKD) 伴高血压患者的诊室血压降低 20.5/8.3 mmHg。事实上,继发于 CKD 的高血压也属于难治性高血压。因此,我们认为两组的血压降低具有可比性,因为入组患者之间存在重叠。另一项研究显示,与缬沙坦相比,盐敏感性高血压患者的血压降低了 13.3/6.2 mmHg,低于我们的结果 13。这可能是因为他们研究中 147.0/90.2 mmHg 的基线血压较低,治疗持续时间较短。缩短 4 周。在我们的研究中,当血管紧张素转换酶抑制剂或血管紧张素受体阻滞剂被沙库巴曲/缬沙坦替代而继续使用其他抗高血压药物时,观察到血压降低。这种新的组合进一步证明了沙库巴曲/缬沙坦在难治性高血压患者中的强大抗高血压功效。
Sacubitril/缬沙坦显着降低难治性高血压患者的诊室和动态血压。 我们的研究为沙库巴曲/缬沙坦治疗难治性高血压提供了新的证据。
原始出处:
Li W, Gong M, Yu Q, Liu R, Chen K, Lv W, Yao F, Xu Z, Xu Y, Song W, Jiang Y. Efficacy of angiotensin receptor neprilysin inhibitor in Asian patients with refractory hypertension. J Clin Hypertens (Greenwich). 2022 Mar 7. doi: 10.1111/jch.14454.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
36
#TENS#
49
相关资讯无法打开网页
44
#缬沙坦#
49
#难治性#
40
#沙库巴曲缬沙坦#
35
#亚洲人群#
60
#ARNI#
51
#高血压#这个研究不错
64