47岁,女性。
因突发剧烈头痛,呕吐,随后意识障碍到急诊室就诊。
查体发现多处淋巴结肿大,左侧乳腺溃疡肿块。GCS 9分,颈强直,Kernig征阳性。多组颅神经损伤。
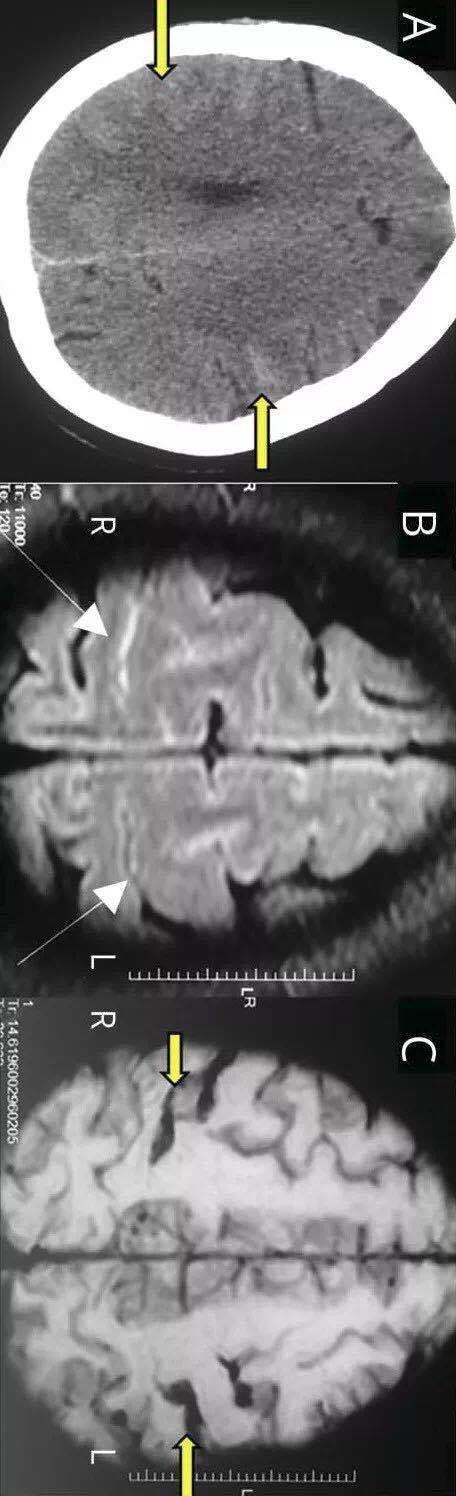
怀疑癌性脑膜炎和出血性软脑膜转移。平扫CT显示双侧顶叶脑沟内SAH(下图A)。CTA未见动脉瘤、血管畸形等。MRI显示双侧顶枕区域SAH(下图B和C),MRV正常。
下图,A图为平扫CT,显示双侧顶枕脑沟内出血(黄色箭头)。B图为Flair(白色箭头),C图为SWI(黄色箭头)显示双侧顶枕脑沟内出血:
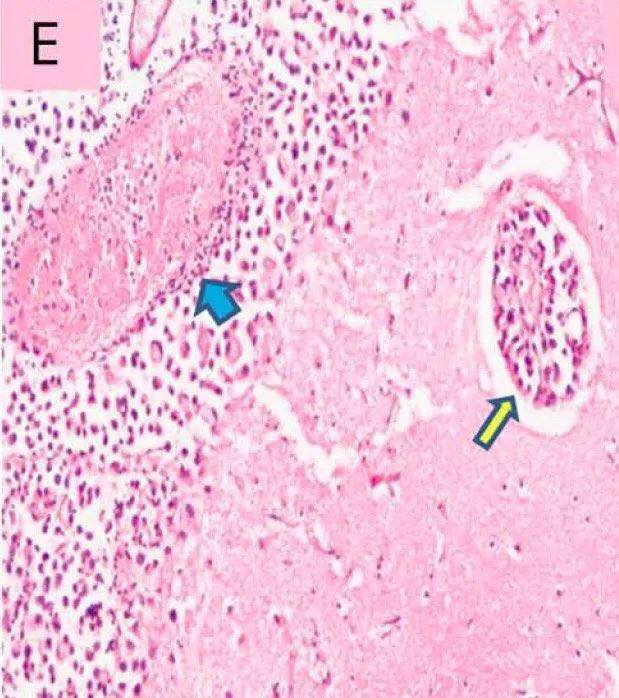
下图D为DSA,显示血管呈串珠样改变(绿色箭头):
脑脊液发现恶性肿瘤,确诊肿瘤性脑膜炎。
乳腺活检为导管浸润癌III级。
入院第4天死亡,随后进行了尸体解剖。
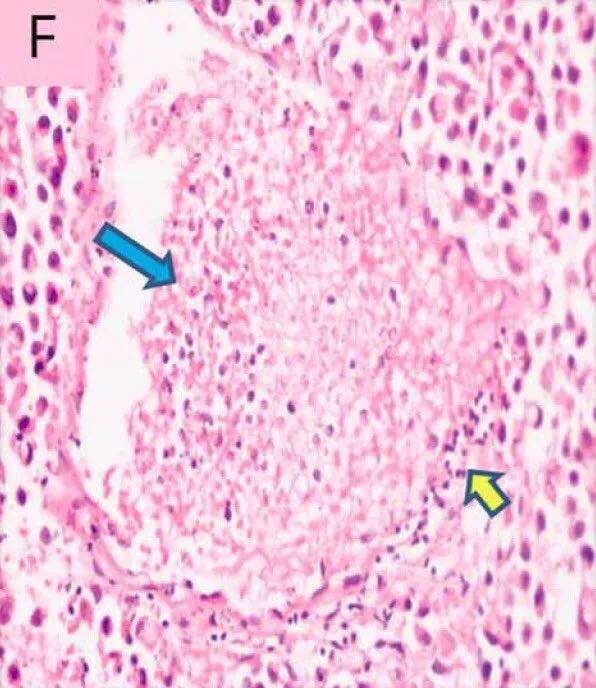
病理证实癌性脑膜炎。血管周围间隙扩大,充满了肿瘤细胞(下图E)。
下图E显示蛛网膜下腔和血管周围间隙(黄色箭头)扩大,充满肿瘤细胞。小血管呈现血管炎表现(蓝色箭头,HE染色):
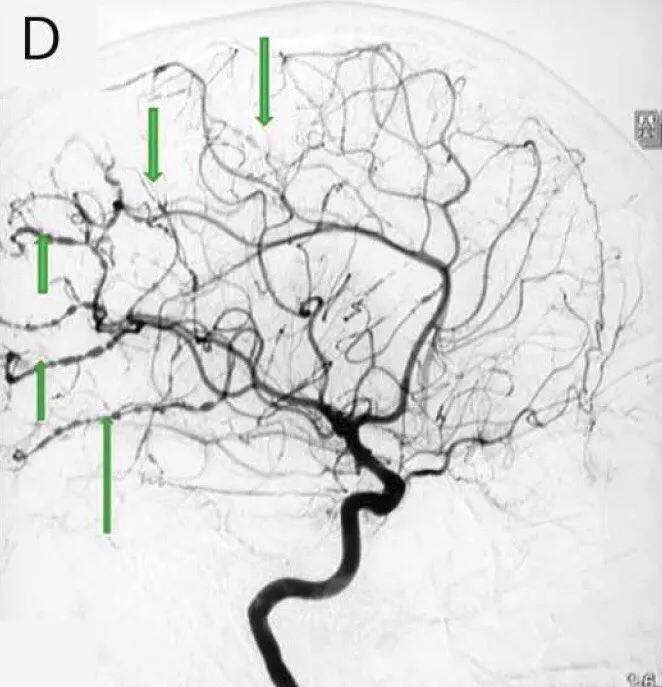
脊膜和神经根广泛肿瘤浸润(infiltration)。Willis环血管的较小分支显示动脉周围浸润(infiltration),内膜炎症和纤维素沉积,无坏死或肉芽肿形成(图F)。
下图F为软脑膜血管血管炎(黄色箭头),合并纤维蛋白血栓形成(蓝色箭头),被肿瘤细胞包围(HE染色):
这些特征符合副肿瘤性血管炎的表现。较大的脑血管被肿瘤细胞包裹(encased),但是无浸润(infiltration)。
作者认为副肿瘤性脑血管炎的病理生理机制包括:1.肿瘤细胞诱导针对血管内皮的免疫反应,2.肿瘤细胞释放各种促炎性因子对内皮的损伤,3.肿瘤蛋白沉积在血管壁上,随后产生迟发性过敏反应,4.含有肿瘤抗原的循环免疫复合物沉积在血管壁上。
原始出处:
Patil A, Shree R, Naheed D, et al. Pearls & Oy-sters: Paraneoplastic cerebral vasculitis: Rare cause of spontaneous convexity subarachnoid hemorrhage. Neurulogy, Feb 27, 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Neurol#
17
学习了谢谢分享!!
58
学习并分享!!
76
#血管炎#
35
作者认为副肿瘤性脑血管炎的病理生理机制包括:1.肿瘤细胞诱导针对血管内皮的免疫反应.2.肿瘤细胞释放各种促炎性因子对内皮的损伤.3.肿瘤蛋白沉积在血管壁上.随后产生迟发性过敏反应.4.含有肿瘤抗原的循环免疫复合物沉积在血管壁上.
75
不错的文章值得拥有
63