European Radiology:究竟如何处理经皮介入手术并发的骨水泥渗漏和错位轴的提取?
2022-09-13 shaosai MedSci原创
在过去几十年中,随着手术数量的增加,开发安全的技术是临床上最重要的目标之一。
 骨水泥成形术是一种微创技术,用于治疗有症状的骨折或机械性损伤的骨病变,在短期和长期随访中都能缓解疼痛。尽管该手术相对安全,但在骨水泥成形术中同样会出现并发症,其中水泥渗漏是最常见的并发症之一,在59.7%的椎体成形术病例中可以观察到,可能引起慢性疼痛,甚至导致治疗失败。
骨水泥成形术是一种微创技术,用于治疗有症状的骨折或机械性损伤的骨病变,在短期和长期随访中都能缓解疼痛。尽管该手术相对安全,但在骨水泥成形术中同样会出现并发症,其中水泥渗漏是最常见的并发症之一,在59.7%的椎体成形术病例中可以观察到,可能引起慢性疼痛,甚至导致治疗失败。
在过去几十年中,随着手术数量的增加,开发安全的技术是临床上最重要的目标之一。已有一些经皮技术实现了这种经皮介入手术复杂化异物的使用,然而目前还缺乏专门关注该主题的大型系列研究。
近日,发表在European Radiology杂志的一项研究评估了大型骨水泥成形术队列中的骨水泥渗漏/锭子拔出率,并进一步描述了可用于提取此类异物的不同经皮策略和技术。
本项回顾性单中心研究纳入了104名接受强化骨水泥成形术的患者和3425名在2012至2020年间接受骨水泥成形术的患者。本研究评估了手术报告和透视图像,以确定手术结果。
6名患者(5.8%)的主轴位置不正,并都在加强型骨水泥成形术中接受了主轴拔出术,成功率为80%。共进行了7次尝试,使用了两种不同的技术。130名患者(32%)在软组织中出现了水泥渗漏,7名(0.6%)在骨水泥成形术中进行了水泥渗漏提取,成功率为100%。共进行了10次尝试,使用了3种不同的技术。没有发生与提取流程有关的重大并发症。
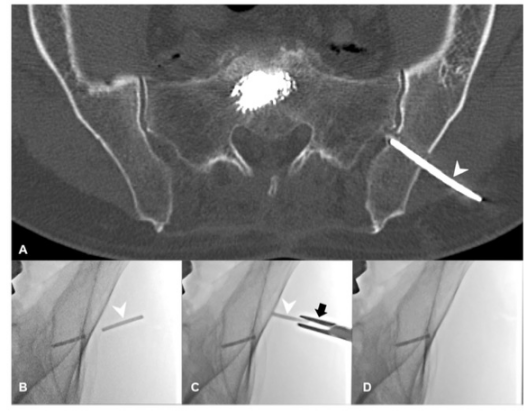
图 一名有症状的骨质疏松性骶骨骨折的64岁男性接受了骶骨成形手术。A 在拔针过程中,一个3厘米长的水泥碎片在臀中肌和皮下组织中漏出(白色箭头)。B 在接下来的日子里,病人遭受了与异物有关的局部疼痛(白色箭头)。C 通过一个小切口插入针架(黑色箭头),在透视下向水泥碎片(白色箭头)推进。D 用针架将水泥碎片抽出后,髂骨外没有水泥残留
本研究发现,骨水泥成形术中主轴错位和骨水泥渗漏的情况并不少见,可进一步导致治疗的失败。本研究涉及的几种经皮技术可以安全、有效地用于取出这种错位的骨轴或水泥渗漏以改善患者的治疗效果。
原文出处:
Pierre-Marie Chiaroni,Kévin Premat,Eimad Shotar,et al.Extraction of cement leakages and malpositioned spindles complicating percutaneous interventions: why, when and how?DOI:10.1007/s00330-022-08787-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#并发#
59
#PE#
46
#介入手术#
44
#骨水泥#
46