Nature:打破自然规律!仅需8个转录因子,干细胞“变身”可受精“卵母细胞”
2020-12-28 探索菌 生物探索
40多年前,世界首例试管婴儿的诞生打破了人类自然孕育生命的历史,为不孕不育患者带来了生育的希望。这之后,辅助生殖技术持续发展,成为越来越多人延续后代和提高生育文明的重要手段。
让不可能变为可能,击破一个个“天命”,似乎是科学家们一直以来乐此不疲、致力追求的目标。
40多年前,世界首例试管婴儿的诞生打破了人类自然孕育生命的历史,为不孕不育患者带来了生育的希望。这之后,辅助生殖技术持续发展,成为越来越多人延续后代和提高生育文明的重要手段。然而,这种技术需要参与者提供健康的精子、卵子,如何精益求精、为不孕不育患者带来更好的解决方案成为科学家们努力的方向。
《Nature》发布了一篇题为“Reconstitution of the oocyte transcriptional network with transcription factors”的报告,为不孕不育患者打破难以生育的“魔咒”带来了全新的希望。
日本九州大学的研究人员通过分析小鼠卵母细胞的发育,揭开了调控卵母细胞生长的基因网络的神秘一角,确定了8个足以触发卵母细胞生长的转录因子。这些转录因子可直接将多能干细胞转化为卵母细胞样细胞,并且转化后的细胞能够像卵母细胞一样受精和分裂。
卵母细胞是女性体内特有的生殖细胞,它的成熟是孕育生命过程的第一步。这种特殊的生殖细胞的细胞质内含有多种混合物质,能够产生200多种人类发育所必须的高分化细胞。
为了了解影响卵母细胞生长的因素,研究人员建立了一个培养系统,利用胚胎干细胞(ES)再现了雌性小鼠生殖细胞的分化,并通过RNA测序(RNA-seq)分析绘制了雌性生殖细胞的发育轨迹,发现有27个转录因子可能与卵母发育过程相关。
其中,仅Lhx8、Sohlh1、Nobox、Tbpl2、Stat3、DYNL1、Sub1以及Figla这8个转录因子是关键因子并且相互影响。其中,Lhx8、Sohlh1、Nobox、Tbpl2形成了一个核心调控网络,而Stat3、DYNL1、Sub1、Figla则紧密相连。
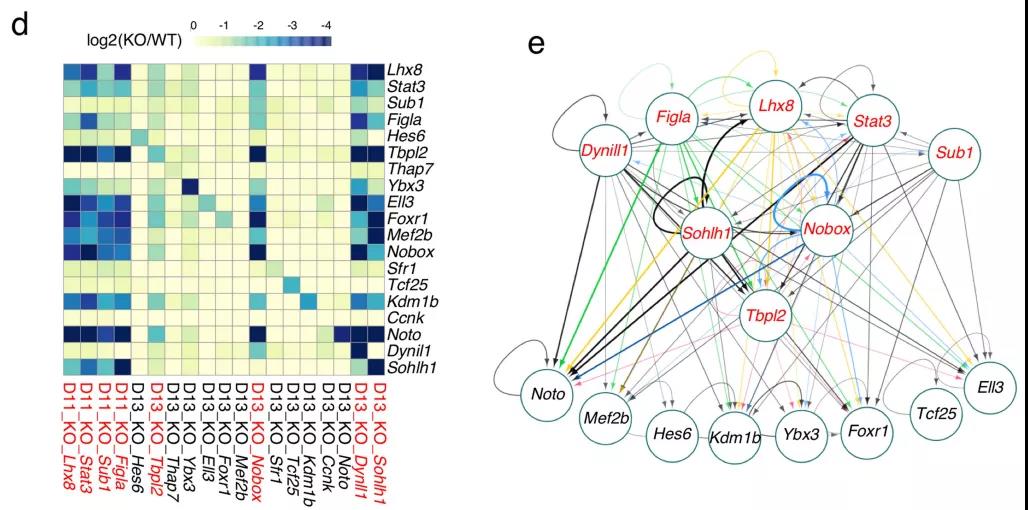
8个转录因子是影响卵母细胞生长的关键因素
于是,研究人员进一步分析了这8个转录因子是否能够诱导小鼠多能干细胞转变为卵母细胞。结果令人惊讶,这些转录因子促成了类卵细胞的产生。研究人员将这些细胞命名为“直接诱导的卵母细胞样细胞”(directly induced oocyte-like cells,DIOLs),尽管这些细胞没有进行减数分裂,但是却能够受精,并能分裂到胚胎发育的8细胞阶段,在这之后发育就会受到影响。
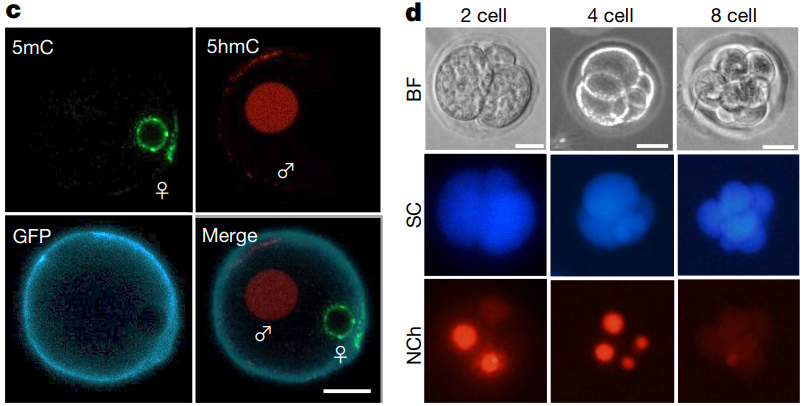
DIOLs能够受精并发育至8细胞阶段
九州大学医学部教授Katsuhiko Hayashi说:“来自卵母细胞的细胞质是生殖生物学和医学中的宝贵资源。我们的研究提供了一种无需侵入人体便能得到大量卵细胞的新颖手段,干细胞可以直接转换为卵母细胞样的细胞,而无需遵循自然发生的相同步骤顺序。尽管这一技术应用在人类身上尚且为时过早,但是小鼠实验已经让我们看到了苗头。”
事实上,步入21世纪以来,科学家们已经在辅助生殖领域取得了一系列重大突破。早在2003年,Hans R. Scholer在《Science》发表了一项开创性的研究报告,提出小鼠胚胎干细胞(ESC)可体外经诱导分化产生卵子样细胞,在学术界引起了一阵轰动。
2016年,中国科学家首次实现小鼠胚胎干细胞体外分化并获得具有功能的精子(样)细胞,同时借助辅助生殖手段使之孕育出健康的小鼠后代,为无精子症男性生育后代带来希望。相关报告发表在干细胞权威杂志《Cell Stem Cell》上。
随着研究的持续推进,“人造卵子”、“人造精子”等技术的不断成熟,未来难以生育的人们将面临更多的治疗选择。或许有朝一日,男性和女性独自孕育后代也将成为现实。
原始出处:
Nobuhiko Hamazaki, Hirohisa Kyogoku, Hiromitsu Araki, et al.Reconstitution of the oocyte transcriptional network with transcription factors.Nature. 2020 Dec 16. doi: 10.1038/s41586-020-3027-9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#转录#
39
进步
69
#Nat#
30
干细胞是热点,但是进入临床仍然需要时间和临床疗效验证哦
37
#转录因子#
40
#受精#
38
#卵母细胞#
36
哇塞
77
学习可
89
学习了
68