Circulation:心肌梗死后接种流感疫苗的疗效分析
2021-08-31 MedSci原创 MedSci原创
与安慰剂相比,在MI或高危冠心病后早期接种流感疫苗可降低全因死亡、MI或支架血栓形成的复合风险,以及可降低12个月时的全因死亡和心血管死亡风险。
观察性和小型随机研究表明,流感疫苗可能会减少心血管疾病患者的心血管事件。

近日,心血管领域权威杂志Circulation上发表了一篇研究文章,研究人员进行了一项由研究者发起的随机双盲试验,以比较灭活流感疫苗与生理盐水作为安慰剂在心肌梗死(MI)(99.7%的患者)或高危稳定型冠心病(0.3%的患者)患者中的疗效。该研究的主要终点为12个月时全因死亡、心肌梗死或支架内血栓形成的复合终点。研究人员对关键次要终点使用分层评估策略:全因死亡、心血管死亡、MI和支架血栓形成。
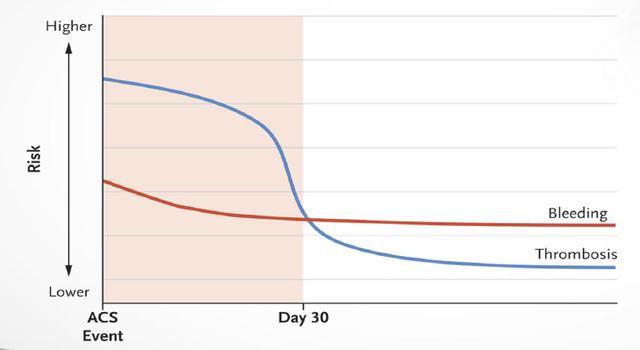
由于Covid-19大流行,数据安全和监测委员会决定在达到预先指定的样本量之前停止试验。2016年10月1日至2020年3月1日期间,2571名参与者被随机分配到8个国家的30个中心;1290人分配接种流感疫苗,1281人分配接种安慰剂。在12个月的随访中,67名(5.3%)接种流感疫苗者和91名(7.2%)注射安慰剂者发生了主要终点(风险比为0.72;95%置信区间为0.52至0.99;P=0.040)。
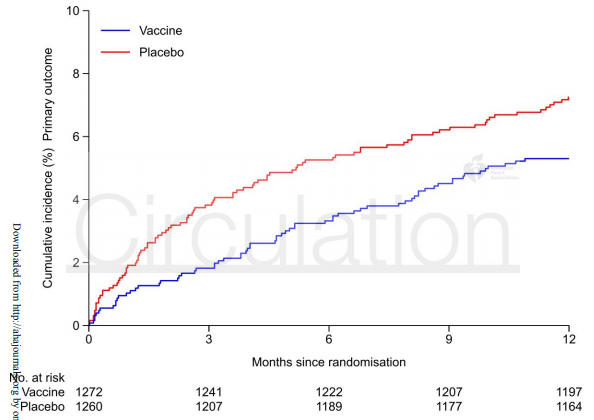
流感疫苗组和安慰剂组的全因死亡率分别为2.9%和4.9%(风险比为0.59;0.39至0.89;P=0.010),心血管死亡率分别为2.7%和4.5%(风险比为0.59;0.39至0.90;P=0.014),流感疫苗组和安慰剂组的MI分别为2.0%和2.4%(风险比为0.86;0.50至1.46,P=0.57)。
由此可见,与安慰剂相比,在MI或高危冠心病后早期接种流感疫苗可降低全因死亡、MI或支架血栓形成的复合风险,以及可降低12个月时的全因死亡和心血管死亡风险。
原始出处:
Ole Frøbert,et al.Influenza Vaccination after Myocardial Infarction: A Randomized, Double-Blind, Placebo-Controlled, Multicenter Trial.Circulation. 2021.https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.121.057042
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效分析#
31
学习了,谢谢分享
67
学习了
56
谢谢梅斯提供这么好的信息,学到很多
63
继续保持
66
好棒
70
不错
40