口服抗乙肝病毒药物中国上市20周年:从疾病预防到治愈还有多远?
2019-11-12 不详 美通社
作为首批进入中国的跨国药企之一,葛兰素史克(GSK)始终以科学为导向,不断创新,将世界领先的药物和产品引入中国,目前,已在中国注册19款药品。在第二届中国国际进口博览会(以下简称“进博会”)上,GSK全方位展现了在呼吸、疫苗、肝炎、HIV/艾滋病、免疫系统疾病、罕见病与中枢神经系统、消费保健品等领域的创新实力与最新研发成果。 GSK首次作为展商参加进博,展现其扎根中国对中国公共卫生作出的重要贡献,
作为首批进入中国的跨国药企之一,葛兰素史克(GSK)始终以科学为导向,不断创新,将世界领先的药物和产品引入中国,目前,已在中国注册19款药品。在第二届中国国际进口博览会(以下简称“进博会”)上,GSK全方位展现了在呼吸、疫苗、肝炎、HIV/艾滋病、免疫系统疾病、罕见病与中枢神经系统、消费保健品等领域的创新实力与最新研发成果。 GSK首次作为展商参加进博,展现其扎根中国对中国公共卫生作出的重要贡献,同时,以“口服抗乙肝病毒药物中国上市20周年”为主题,展现了其对中国乙肝防治的长期承诺。
探索乙肝创新型疗法,在研新药II期临床结果喜人
据数据显示,目前全球有超过2.5亿乙肝病毒感染者,而中国占了其中的1/3。慢乙肝是一种由乙肝病毒感染引起的疾病,导致肝脏炎症、肝硬化,肝脏失代偿以及肝癌。中国的乙肝病毒感染多为B、C基因型,C基因型感染慢乙肝进展为肝癌的比率更高。目前,对慢性乙肝的治疗主要是最大限度的抑制HBV复制,减轻肝细胞炎性坏死及肝纤维化,延缓和减少肝功能衰竭、肝硬化失代偿、HCC及其他并发症的发生,从而改善生活质量和延长生存时间,然而想要实现功能性治愈,需要更多的临床新药的研发。
据悉,近期GSK宣布了与Ionis制药公司合作开发治疗乙肝的创新药物。该新药是第二代肝靶向反义寡核苷酸,一项Phase 2a 期临床研究正在评估其安全性,耐受性和药代动力学(PK)。在近期公布的部分临床试验结果中,该药物体现出可接受的安全性,并表现出靶标参与伴随HBsAg平均下降呈剂量依赖性。
GSK中国医学事务负责人、副总裁贺李镜博士表示:“该靶向乙肝病毒基因表达的创新疗法已在II期临床试验中获得积极结果,有望为患者提供一种持久的、变革性的疗法,希望离‘功能性治愈乙肝’的目标越来越近。同时,受惠于目前中国政府非常开放的审评机制,使得在科研方面的投入和新药进入中国市场的步伐得以大大加快。因此这款药物在中国的研发工作几乎是和美国同时进行的。”
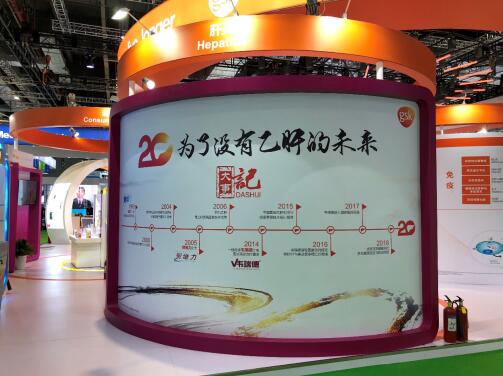
20周年路线图勾勒出GSK对中国乙肝防治的长期承诺
今年是GSK第一款口服抗乙肝病毒药物在国内上市的20周年。在过去的20年里,GSK一直牢记使命,不忘初心,致力于乙肝的防治工作。1999年,GSK国内上市第一款口服抗病毒药物“贺普丁”。2004年,研究结果证实口服抗病毒治疗能延缓慢乙肝疾病进展。2005年,GSK上市了第二款口服抗病毒药“贺维力”。2010年,在全国24个中心启动慢乙肝联合治疗 Explore研究,共同对抗耐药问题。2014年,GSK全新一线治疗药物“韦瑞德”上市,更好满足患者需求。
GSK中国肝炎业务部负责人孙蕾女士表示:“从20年前在中国上市首个口服抗乙肝病毒药物,到现在拥有涵盖从疫苗到抗病毒治疗药物的领先产品组合,GSK不断将最先进的产品和治疗方案引入中国市场,始终致力于提升高效口服抗乙肝病毒药物及相关规范化治疗手段的可及性,帮助更多中国的乙肝患者获得规范化的乙肝抗病毒治疗。”
GSK着眼于患者的未尽之需,创新不停,建立起覆盖从预防到治疗全程的疾病管理解决方案。秉承帮助人们“做到更多,感觉更舒适,生活更长久”的理念。同时,GSK亦致力于让乙肝规范化抗病毒治疗覆盖到更深、更广、更需要的地区和人群中去,不断提高药物可及性,为提升基层疾病认知和诊疗水平提供全面支持,助力中国乙肝防治工作。
据悉,2015年和2018年,GSK参与两项由卫生管理部门所组织的基层乙肝防治项目:中国基层乙肝防治与健康管理技术培训项目和扶贫攻坚健康同行 – 肝炎健康促进与防治项目。中国基层乙肝防治与健康管理技术培训项目历时730天,走过31个省市58个城市,开展了58场培训班,共有9248名区县级临场医生参加了现场培训。另外,自扶贫攻坚 健康同行——肝炎防治与健康促进项目开展以来,共主办15场次的下基层活动,为2000余名基层患者和群众提供义诊咨询服务,有近千名基层医生接受乙肝防治的临床技术指导。
着眼乙肝防治挑战,探索防控新模式
近年来,乙肝一直位居我国法定传染病发病率的前三位,给中国的患者、社会和卫生医疗系统带来沉重的经济负担。世界卫生组织提出“到2030年要消灭病毒性肝炎”的目标,实现乙肝治愈,一直是世界医疗健康行业所关注的方向。然而,为了实现2030目标,我们还面临着很大的挑战,我国乙肝诊断和治疗的覆盖率距离实现2030目标的差距最大。2016年我国得到乙肝诊断的比例仅为18.7%,得到乙肝治疗的比例仅为10.8%。因此,提高我国乙肝诊断和治疗的覆盖率将成为我国乙肝防治的重要目标。
回顾我国20年来的肝炎防治进程,海军军医大学905医院临床肝病研究中心主任、主任医师陈成伟教授表示,“我国政府一直以来都高度重视肝炎防治工作,通过预防和治疗两大抓手有力推进乙肝防治工作,近年来新发慢性乙肝病毒感染率已经大幅度降低。但作为乙肝大国,我国乙肝防治仍然面临严峻挑战,现有慢性乙肝病毒感染人数仍然众多,患者知晓率、抗病毒治疗药物的可及性及规范抗病毒治疗率都有待提高,下一步需要建立起集预防-筛查-诊断-治疗为一体的完整乙肝防控体系。”
最后,GSK新兴市场高级副总裁Fabio Landazabal先生表示,“作为长期深耕乙肝和抗病毒治疗领域的领先企业,GSK在乙肝治疗领域拥有丰富经验。在持续研发创新药品的基础上,提升基层医疗水平和疾病认知、不断扩大药品可及性,为患者提供更多治疗选择也将在中国的乙肝防治中发挥重要作用。未来我们将携手行业合作伙伴,继续为基层医疗水平提升提供全面支持。同时我们也在积极探索‘互联网+医疗’创新模式,努力提高我们药品的可及性,最大限度方便患者选择符合其需求的治疗方案。让我们共同为消除乙肝、实现‘健康中国2030’愿景不懈努力。”
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#抗乙肝病毒药物#
29
非常受益,很好的研究
62
非常受益,很好的研究
61
非常受益,很好的研究
72
非常受益,很好的研究
69
非常受益,很好的研究
61
非常受益,很好的研究
28
非常受益,很好的研究
19