JACC:左心室心肌不紧合患者的临床心血管事件风险的预测
2021-08-13 Nebula MedSci原创
左心室心肌不紧合与心力衰竭和室性心律失常风险增加独立相关
左心室心肌不紧合(LVNC)是一种罕见的发育不良性心肌病,可发生心衰、严重的心律失常或血栓栓塞,可以发生于在任何年龄,其特征是心肌小梁突出,病因及其预后均尚未明确。
该研究目的是开发并验证主要心血管不良事件(MACE)的预测模型,并在长期随访过程中识别无事件的LVNC病例。
这是一项回顾性的、纵向、多中心队列研究,研究对象是通过超声心动图或心血管磁共振检查达到LVNC标准的患者。MACE定义:心力衰竭(HF)、室性心律失常(VA)、全身栓塞或全因死亡。
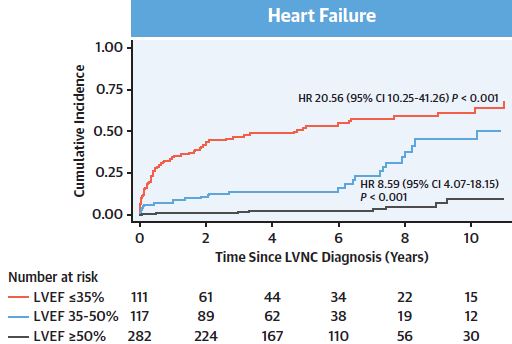
根据LVEF分层的患者HF和VA的累积发生率
共纳入了585位患者(45±20岁,57%的男性)。左室射血分数(LVEF)为48%±17%,18%的患者存在晚期钆增强(LGE)。中位随访了5.1年后,223位(38%)患者发生了MACE:HF 110例(19%)、VA 87例(15%)、全身栓塞 18例(3%)和死亡 24例(6%)。LVEF是与MACE独立相关的主要变量(p<0.05)。LGE与LVEF>35%的患者的HF和VA风险相关(p<0.05)。
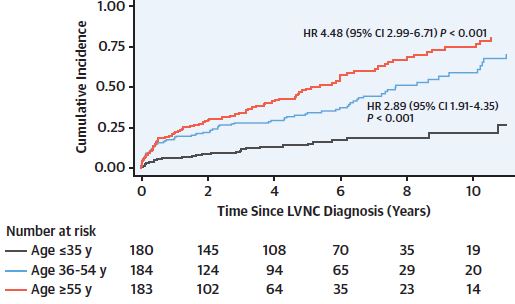
根据年龄分层的患者MACE事件的累积发生率
研究人员采用Cox回归分析建立了MACE的预测模型,纳入了年龄、性别、心电图、心血管风险因素、LVEF和家族聚集性因素。该预测模型在开发队列和外部验证队列中的C-指数都是0.72。无心电图异常、LVEF≥50%、无LGE和家族筛查阴性的患者在随访过程中未发生一例MACE。
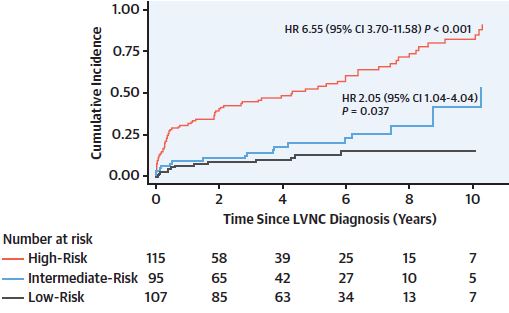
根据模型预测风险分层的患者的MACE事件的累积发生率
总而言之,LVNC与心力衰竭和室性心律失常风险增加独立相关。LVEF是与MACE独立相关性最强的变量;但是,LGE会使没有严重收缩功能障碍的患者发生MACE事件的风险额外增加。最后,该研究开发的预测模型或有助于指导这类患者的临床管理。
原始出处及参考文献:
[1]Guillem Casas, et al. Clinical Risk Prediction in Patients With Left Ventricular Myocardial Noncompaction. J Am Coll Cardiol. 2021 Aug, 78 (7) 643–662
[2]汪洁, 陈树宝, 孙锟,等. 左室心肌不紧合的二维超声心动图诊断[J]. 中国医学影像技术, 2002, 018(007):663-664.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#临床心血管#
28
#JACC#
24
#血管事件#
35
需要系统学习
55
#心血管事件风险#
47
#ACC#
26
#左心室#
47
棒棒棒👍🏻
62