Plast Reconstr Surg:烧伤后慢性神经痛,一种解剖学方法以及预测患者风险的模型的开发和验证
2021-10-31 MedSci原创 MedSci原创
据报道,烧伤相关神经疼痛的患病率在6%到82%之间。烧伤医生对烧伤伤口部急性疼痛的适当药物治疗有着全面的了解,但烧伤后神经疼痛的慢性表现尚不清楚。慢性疼痛定义为从烧伤中心出院后持续6个月或6个月以上的
据报道,烧伤相关神经疼痛的患病率在6%到82%之间。烧伤医生对烧伤伤口部急性疼痛的适当药物治疗有着全面的了解,但烧伤后神经疼痛的慢性表现尚不清楚。慢性疼痛定义为从烧伤中心出院后持续6个月或6个月以上的疼痛。
以前关于与解剖位置无关的烧伤相关神经痛的危险因素的报告包括年龄超过20岁、全身表面积烧伤百分比超过20%、全身烧伤、危重病、电损伤和酗酒。
烧伤位置可以确定是否有发生烧伤相关神经痛的风险。如果可以预测烧伤患者发生烧伤相关神经痛的风险,在烧伤治疗的急性期早期进行选择性医疗或外科治疗可能会改善患者的预后。
该研究的目的是确定涉及身体不同解剖部位的烧伤患者的特征,以确定解剖特定的危险因素,然后开发并验证一个基于数学方程的模型,主要将患者分为11个解剖烧伤部位进行比较(即手、前臂、上臂、胸部/腹部、后身、臀部/生殖器、大腿、小腿、脚、面部/头部、颈部)比较发生和未发生烧伤相关神经痛的患者的每个解剖烧伤部位。
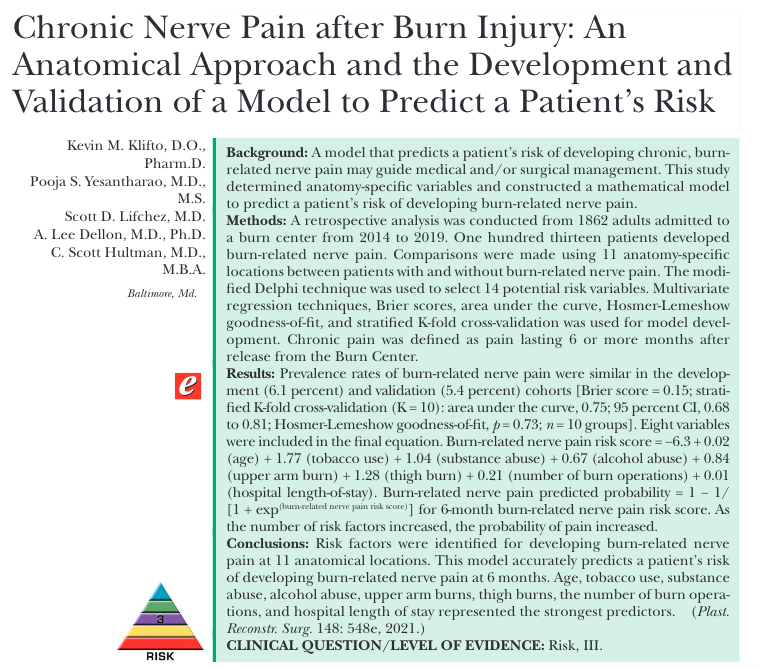
图1文章来源截图
该研究对2014年至2019年间入住烧伤中心的1862名成年人进行回顾性分析并进行模型开发。其中113名患者出现烧伤相关神经痛。故研究人员在有和没有烧伤相关神经痛的患者之间,使用11个解剖位置进行比较。

图2 11个解剖位置
结果显示,在发展(6.1%)和验证(5.4%)队列中,烧伤相关神经疼痛的患病率相似。
最终方程中包括八个变量。公式如下:
烧伤相关神经疼痛风险评分=−6.3+0.02(年龄)+1.77(吸烟)+1.04(药物滥用)+0.67(酒精滥用)+0.84(上臂烧伤)+1.28(大腿烧伤)+0.21(烧伤手术次数)+0.01(住院时间)。烧伤相关神经痛预测概率=1− 1/[1+exp(烧伤相关神经疼痛风险评分)]
这可用于6个月的烧伤相关神经疼痛风险评分。
除此外,随着危险因素数量的增加,疼痛发生的可能性增加。
最终,研究人员在11个解剖部位确定了发生烧伤相关神经疼痛的危险因素,并研发出相关模型。该模型准确预测了患者在6个月时发生烧伤相关神经痛的风险。年龄、吸烟、药物滥用、酒精滥用、上臂烧伤、大腿烧伤、烧伤手术次数和住院时间是最强的预测因子。
原始文章:
Klifto Kevin M,Yesantharao Pooja S,Lifchez Scott D et al. Chronic Nerve Pain after Burn Injury: An Anatomical Approach and the Development and Validation of a Model to Predict a Patient's Risk.[J] .Plast Reconstr Surg, 2021, 148: 548e-557e.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#NST#
41
#AST#
24
#神经痛#
38
#解剖学#
53