“非典型性脂肪瘤”就不危险吗?
2017-09-18 牛晓辉 郝 林 骨肿瘤
脂肪肉瘤影像学上有其特殊表现,B超、X线、CT、MRI各有何优缺点?高分化的脂肪肉瘤有时在临床上被称为“非典型性脂肪瘤”,这就意味着其潜在危险性低吗?
脂肪肉瘤影像学上有其特殊表现,B超、X线、CT、MRI各有何优缺点?高分化的脂肪肉瘤有时在临床上被称为“非典型性脂肪瘤”,这就意味着其潜在危险性低吗?
(1)病例介绍
:患者,女,49岁,主因右下肢间断酸胀不适1年,发现右大腿后侧肿物6个月,下肢酸胀加重10天入院。患者1年前开始无明显诱因间断出现右下肢酸胀不适,休息后好转,无疼痛,无活动受限,未予诊治。6个月前,患者发现右大腿后方包块,无压痛,仍未诊治。10天前患者自觉大腿酸胀症状加重,于外院就诊,发现右大腿后方巨大软组织肿块,为进一步诊治来我院。
入院查体:步行入院,正常步态。右大腿后侧可见肿块,局部颜色正常,皮温增高,无皮肤破溃,可见静脉曲张,肿物约20cm×10cm,质软,有轻压痛,不活动,肿物边界不清,未闻及血管杂音。患侧髌骨上20cm处大腿周径64cm,对侧周径59cm。双侧髋关节、膝关节活动无受限。双侧腹股沟淋巴结未及肿大。
影像学检查:B 超显示右大腿后内侧肌肉内团块、混杂信号。腹股沟淋巴结未见肿大。X 线片显示右股骨未见明显骨质破坏,右股骨侧位X 线片显示股骨后方巨大软组织影,密度低于周围肌肉组织,呈典型的脂肪密度,未见钙化(图26‐1)。CT 显示右大腿后内侧软组织内可见不规则低密度灶,内有分隔,周围可见包膜,测CT 值约-111.6HU,增强扫描未见强化,邻近骨质未见异常(图26‐2)。MRI 显示右大腿中上段股骨后方软组织内可见不规则长T 1长T 2信号影,边界清晰,抑脂像信号减低,肿物大小约19 cm ×11 cm ×7.5cm,骨结构完整,病变位于股二头肌内,将周围肌肉向两侧挤压(图26‐3)。肺CT 显示双侧胸廓对称,气管、支气管通畅。肺纹理走行自然,心脏大小形态正常。纵隔内未见异常肿大的淋巴结影。双肺内未见结节。

图26‐1 X 线片示右股骨未见明显骨质破坏,右股骨侧位X 线片显示股骨后方巨大软组织影,密度低于周围肌肉组织,呈典型的脂 肪密度,未见钙化
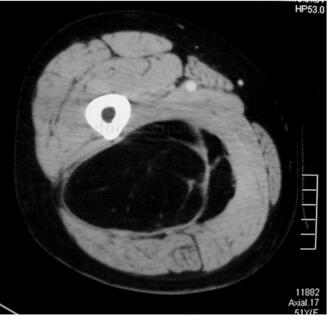
图26‐2 CT 示右大腿后内侧软组织内可见不规则低密度灶,内有分隔,周围可见包膜,测CT 值约-111.6HU,增强扫描未见强化,邻近骨质未见 异常
常规化验正常。行术前肿瘤穿刺活检,病例报告:穿刺标本,脂肪、纤维、血管组织,其中见较成熟脂肪细胞增生,个别脂母细胞。
完善常规检查后,在连续硬膜外麻醉下行右大腿肿瘤切除术。麻醉满意后,患者俯卧位,常规消毒铺巾,大腿后侧正中纵行切口,梭形切除穿刺道周围皮肤及皮下软组织。从大收肌与半腱肌、半膜肌间隙进入,外侧经过外侧肌间隔后进入,内侧沿大收肌外侧分离,坐骨神经位于肿瘤的浅层,与肿瘤之间有分隔,予以保护。见肿瘤位于股二头肌内,在肿瘤外保留薄层正常肌肉包绕肿瘤,将肿瘤切除。冲洗,止血。置入伤口负压引流管,逐层缝合伤口

图26‐3 脂肪肉瘤a﹒右大腿中上段股骨后方软组织内可见不规则长T 1信号影,边界清晰;b、c﹒肿瘤显示为长T 2信号;d﹒抑脂像信号减低
术后病理报告:分叶状肿瘤,脂肪细胞相对成熟,但仍有轻度异型性,大小不一,散在间质内的异型性明显的单核及多核细胞,胞核大,深染,未见典型的脂肪母细胞,考虑为高分化脂肪肉瘤。
术后常规应用抗生素7~10天,24小时引流<25ml 后拔除引流管。
患者术后两周伤口一期愈合拆线出院,术后两周拄拐杖,避免负重下地活动,3周逐渐增加部分负重,至弃拐完全负重活动。
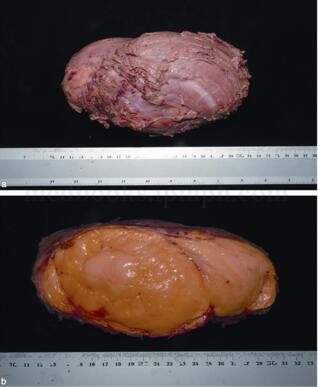
图26‐4 脂肪肉瘤a﹒切除肿瘤标本,肿瘤表面有一薄层肌肉覆盖;b﹒肿瘤剖面图
(2)专家分析
:脂肪肉瘤是仅次于恶性纤维组织细胞瘤的第二常见软组织肉瘤,占10%~20%。该肿瘤好发年龄为40~60岁。男女发病率大致相当。好发于肢体和腹膜后,75%的病例发生在肢体深部组织,20%发生在腹膜后,其余的分布于腹股沟,精索及其他多个部位,其他可能发生脂肪肉瘤的罕见部位包括:口腔,胸壁和纵隔。肿瘤常起源于正常的脂肪组织,例如血管周围或神经周围的脂肪组织。脂肪肉瘤常常直径>5cm,位于深筋膜的深层,极少在皮下组织中出现。
肿瘤的症状与肿瘤的部位有关,在肢体表现为缓慢生长的包块,在患者就诊前常有数月至数年的病史。发生在腹膜后的脂肪肉瘤常常伴随普通的腹内包块症状。高分化脂肪肉瘤含有典型的成熟脂肪成分,因此影像学上表现为脂肪密度的包块,在相应的纤维化和硬化区可见花斑状或者条纹状密度影,其界限没有脂肪瘤清晰。
该患者为中年女性,处于脂肪肉瘤的高发年龄段,患者病史1年,X 线片及CT 上呈现典型的脂肪密度,MRI 上呈现典型的脂肪信号。根据术前病理活检,可明确肿瘤为脂肪来源。虽然没有明确报告为脂肪肉瘤,但肿瘤位于深筋膜深层,直径大于5cm,这都是诊断软组织恶性肿瘤的重要依据。因此结合术前临床表现、影像学表现及病理结果,首先应考虑高分化脂肪肉瘤诊断。
(3)诊断要点
:脂肪肉瘤影像学上有其特殊表现。B 超检查简单方便,价格便宜,无创伤,是显示软组织肿瘤很好的方法,可确定肿瘤的位置、数量、大小,是否有分叶,囊性或实性。
在X 线片上,绝大多数脂肪肉瘤的密度与邻近的肌肉相似,X 线上几乎没有特征可以将脂肪肉瘤与其他软组织肉瘤相区别。罕见的骨内脂肪肉瘤具有侵袭性病变的特征,表现为密度减低的穿透样破坏区,但此表现并不能提示病变的组织发生。X 线片上的钙化可见于脂肪瘤、异位骨化、滑膜肉瘤、血管瘤及软骨瘤等。
像所有的软组织肉瘤一样,同位素扫描的早期血管相显示:与邻近正常组织相比病变区有局灶性的摄取量增加。但在晚期骨骼相中,经常可见脂肪肉瘤的同位素摄取量几乎比其他所有的软组织肉瘤都高。据推测,这种摄取量升高是由于脂肪肉瘤中含有大量离子钙。这种同位素摄取增加具有一定的规律性,足以提示其组织发生,但不总是可靠的。
脂肪肉瘤是一种高血运病变,在血管造影的早期动脉相和晚期静脉相中,明显可见高血运状态。但是没有独特的血管造影特征可将脂肪肉瘤与其他软组织肉瘤区别开来。
CT 图像比传统X 线片能更清楚地显示脂肪肉瘤的边界。病变密度常常比周围肌肉的低,虽然这种低密度不如脂肪瘤那么明显,但也常比其他软组织肉瘤低,足以提示其组织发生。注射造影剂可使病变的CT 图像强化,反映出病变的高血运状态,同血管造影术所显示的一样。
MRI 是显示巨大软组织肿物的最好方法,可显示肿物与周围神经血管结构的关系,在恶性纤维组织细胞瘤中可以显示出黏液、血管和纤维成分。在MRI 上,脂肪肉瘤与脂肪瘤表现相似。MRI 有助于评价肿块的范围和间室情况,但在确定肉瘤的组织发生类型上作用有限。
病理方面,大体标本上可见肿块被包膜包裹,并且很容易从周围结构分离开。与高度恶性的多形性脂肪肉瘤相比,这种现象在低度恶性的黏液型脂肪肉瘤更明显。两者均表现为分叶状。黏液型脂肪肉瘤的切面呈柔软的黏液瘤样组织。偶尔有些病变主要由成熟的脂肪细胞构成,肿瘤组织很容易被辨认为脂肪。而比较常见的病变主要由不成熟的脂肪母细胞构成,表现为富含血管的组织。多形性脂肪肉瘤常表现为浸润性生长并富含脂肪。肿瘤内经常有明显的囊性退变和出血区,而在黏液型中这种现象是不常见的。在这两种类型的脂肪肉瘤的周围均常见卫星灶。
镜下组织学表现为在黏液瘤样不定形基质中散布成片的脂肪细胞和(或)脂肪母细胞,细胞、基质之比较小。肿瘤组织中含有大量纤细的毛细血管分支,呈独特的树枝状,在低倍镜下观察,肿瘤组织特别像道路图。
脂肪肉瘤有数种组织亚型:去分化型、黏液型、多形性型、脂肪瘤样型、圆细胞型及混合型等。但主要类型有两种:①黏液型脂肪肉瘤(大约占所有脂肪肉瘤的50%),一般是低度恶性的Ⅰ期病变;②多形性型脂肪肉瘤(大约占所有脂肪肉瘤的30%),通常是高度恶性的Ⅱ期病变,但有个别例外。
脂肪肉瘤仅对S‐100 抗原染色阳性,但是软骨、神经性以及肌肉起源的肉瘤也同样对S‐100 抗原染色呈阳性,因此S‐100 阳性染色并不能特异性地诊断脂肪肉瘤。
遗传学上,高分化脂肪肉瘤可出现环状和巨染色体,这些标志性染色体内含有包括MDM2 基因的12q14‐15 区域的扩增。
(4)治疗原则
:脂肪肉瘤的治疗原则是手术切除和辅助放疗。脂肪瘤和高分化脂肪肉瘤通常行边缘切除,高分化脂肪肉瘤以及异型性明显的脂肪类肿瘤复发率高,达20%~25%,因此需要密切随访,监测是否复发。对黏液型、多形性型脂肪肉瘤以及其他少见的组织亚型的治疗是相同的。
手术治疗遵循软组织肉瘤的一般处理原则。低度恶性的Ⅰ期病变(大多数黏液型脂肪肉瘤),可行广泛切除或经满意的术前放疗后行边缘切除。Ⅱ期高度恶性者需根治性切除或经满意的术前放疗后行广泛切除。放疗被用于术前以辅助保肢手术,这样做可以使手术切除范围较小,从而获得较好的肢体功能。
肉瘤的化疗一般用于Ⅲ期已有转移的患者,或者用于低分化脂肪肉瘤的治疗。经过充分治疗的黏液型脂肪肉瘤的5年生存率约为90%,而多形性型脂肪肉瘤约为60%。若手术切除的外科边界足够,则局部复发率小于10%。脂肪肉瘤有一个独一无二的特点,即下肢的病变得到控制之后,在腹膜后出现第2个病变的发生率为30%~50%,然而第2个病变属原发还是继发尚未可知。

图26‐5 术后3年复查,肿瘤局部无复发
(5)随诊结果
:该患者术后每3个月随访1次,目前术后随访3年,肿瘤无复发及转移(图26‐5)。患者可步行,步态正常。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#非典型性#
42
学习了.谢谢分享
76
#脂肪瘤#
50
#非典型#
44
谢谢分享.超厉害的说
84
学习了很有用不错
93