European Radiology:在非小细胞肺癌患者中,我们又发现了一个强有力的影像学预后标志物
2022-04-16 shaosai MedSci原创
目前的指南推荐使用[18F]FDG PET/CT对所有NSCLC患者进行初始分期。
 据统计,肺癌是全世界范围内最常见的恶性肿瘤之一,占癌症死亡人数的比例最高。非小细胞肺癌(NSCLC)是肺癌最常见的组织学亚型(占所有病例的70-85%),主要有两种组织学类型:腺癌(ADC)和鳞状细胞癌(SCC)。然而,即使进行了根治性切除手术,但仍有20%至52%的I-III期患者出现局部复发或远处转移。
据统计,肺癌是全世界范围内最常见的恶性肿瘤之一,占癌症死亡人数的比例最高。非小细胞肺癌(NSCLC)是肺癌最常见的组织学亚型(占所有病例的70-85%),主要有两种组织学类型:腺癌(ADC)和鳞状细胞癌(SCC)。然而,即使进行了根治性切除手术,但仍有20%至52%的I-III期患者出现局部复发或远处转移。
目前的指南推荐使用[18F]FDG PET/CT对所有NSCLC患者进行初始分期。从患者治疗前的[18F]FDG PET/CT扫描中获得的定量变量的潜在用途一直是许多研究的重要方向。
经典的PET变量,如基于标准化摄取值(SUV)和基于体积的变量,如代谢性肿瘤体积(MTV)和病变总糖酵解(TLG),已被多项研究作为预测预后的重要因素,但结果并不一致。最近,文献中出现了基于测量肿瘤几何特征的新方法来寻找预测预后的新的指标。
近日,发表在European Radiology杂志的一项研究探讨了两个新的几何变量,即由治疗前[18F]FDG PET/CT获得的归一化SUVpeak到中心点距离(nSCD)和归一化SUVmax到周边距离(nSPD)的预后价值,并与接受手术的NSCLC患者的经典代谢参数的相关性进行了比较。
本项回顾性研究纳入了具有基线[18F]FDG PET/CT的I-III期NSCLC患者,并获得了每位患者的临床、组织病理学和代谢参数。对肿瘤进行分割并获得了SUV和基于体积的变量、纹理、球形度和两个新的参数,即归一化SUVpeak到中心点距离(nSCD)和归一化SUVmax到周边距离(nSPD)。早期复发(ER)和短期死亡率(STM)作为研究终点。对ER和STM进行了单变量的逻辑回归和多变量的逻辑回归。
本研究共纳入了173名患者。在49/104名复发患者中检测到ER。此外,100名患者死亡,53名有STM。年龄、病理淋巴管侵犯、淋巴结浸润、TNM分期、nSCD和nSPD与ER相关,但在多变量分析中只有年龄(aOR = 1.06,p = 0.002)、病理淋巴管侵犯(aOR = 3.40,p = 0.022)和nSPD(aOR = 0.02,p = 0.018)是ER的重要独立预测因素。年龄、淋巴结浸润、TNM分期、nSCD和nSPD是STM的预测因素。在多变量分析中,年龄(aOR = 1.05,p = 0.006)、淋巴结浸润(aOR = 2.72,p = 0.005)和nSPD(aOR = 0.03,p = 0.022)与STM显著相关。变异系数(COV)和SUVmean/SUVmax比率对ER或STM没有显示出明显的预测价值。
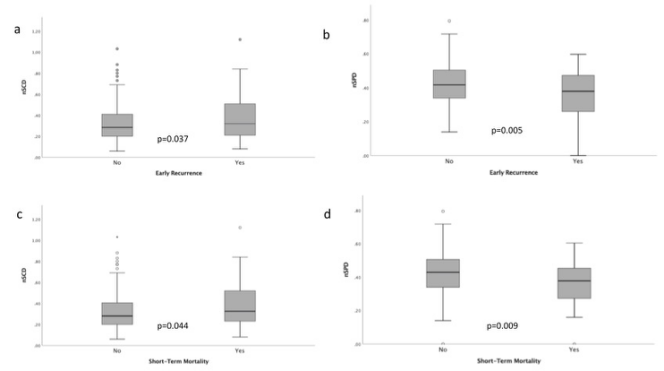
图 nSCD和nSPD与早期复发(a, b)和短期生存(c, d)之间的关系
本研究结果表明,nSCD和nSPD可作为预测NSCLC患者预后较差的预测指标,其表现优于经典的PET衍生变量。这两个参数都能识别出具有高风险的ER和STM的患者。本研究提示,将这些新的变量与临床和病理因素一起,将有助于临床建立适应风险的治疗策略。
原文出处:
Germán Andrés Jiménez Londoño,Ana Maria García Vicente,Jesús J Bosque,et al.SUVmax to tumor perimeter distance: a robust radiomics prognostic biomarker in resectable non-small cell lung cancer patients.DOI:10.1007/s00330-021-08523-3
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非小细胞#
55
#标志物#
54
#预后标志#
48
#PE#
38
#肺癌患者#
56
#预后标志物#
38
#非小细胞肺癌患者#
46