World J Urol:miR-3195、miR-3687和miR-4417的上调与去势抵抗性前列腺癌相关
2021-05-27 AlexYang MedSci原创
前列腺癌是男性生殖系统最常见的恶性肿瘤,其发病率和死亡率在欧美国家仅次于肺癌,位居男性癌症死亡的第2位。2014年,仅美国即新增前列腺癌患者233000人,死亡29480人,而2016年北美地区前列腺
前列腺癌是男性生殖系统最常见的恶性肿瘤,其发病率和死亡率在欧美国家仅次于肺癌,位居男性癌症死亡的第2位。2014年,仅美国即新增前列腺癌患者233000人,死亡29480人,而2016年北美地区前列腺癌预测新发病例约180890,占所有男性新发实体肿瘤总数的21%,且据预测,2023年前列腺癌治疗市场规模将增长至83亿美元。目前,尽管我国前列腺癌的发病率明显低于欧美,但是近10年来,由于社会老龄化、人口城市化、膳食结构西方化及血清前列腺特异性抗原(PSA)筛查的逐步推广,其发病率快速增长,正日益成为严重威胁我国男性健康的疾病。

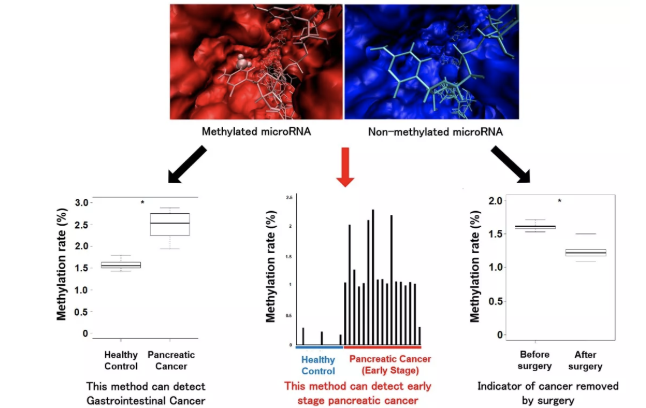
前列腺癌(PCa)是癌症相关死亡的一个主要原因。雄激素阻断治疗后,该疾病可能进一步发展为去势抗性PCa(CRPC),且预后不佳。微核糖核酸(miRNAs)是一类小的非编码RNAs,在基因调控中发挥着关键作用。
近期,有研究人员分析鉴定了与CRPC相关的miRNAs,并评估了它们的功能作用。
在这项研究中,共包括了23个良性前列腺增生症(BPH)样本、76个原发性PCa样本和35个CRPC样本。研究人员从组织切片中提取总RNA,并在Affymetrix GSC 3000平台上进行miRNA谱分析。随后,进行茎环结构RT-qPCR分析验证所选miRNA的表达水平。之后,研究人员使用用miRNA类似物或抑制剂转染PCa细胞系,评估其对细胞增殖、细胞迁移和细胞侵袭的影响。
在分析研究中,他们发现与原发性PCa组织相比,CRPC中的几个miRNAs表达失调,其中miR-205(-4.5倍;p=0.0009)、miR-92b(-3. 1倍;p<0.0001)下调;miR-3195(+5.6倍;p<0.0001)、miR-3687(+8.7倍;p=0.0006)和miR-4417(+5.0倍;p=0.0005)上调。虽然KLK3、miR-21和miR-141在雄激素处理的VCaP和LNCaP细胞中的表达水平有所增加,但miR-3687和miR-4417的表达水平却有所下降。在AR阴性的PC3细胞系中,没有一个miRNA是受雄性激素调控的。miR-3687的过量表达减少了细胞迁移和细胞侵袭,而miR-3195的过量表达增强了细胞迁移。

miR-205、miR-3195、miR-3687和miR-4417的表达以及与CRPC的相关性
综上所述,他们在CRPC组织中发现了几个新的失调的miRNAs,包括了两个可能参与肿瘤侵袭的miRNAs。他们的数据支持了miRNAs参与PCa肿瘤发生和发展为CRPC过程的假设。但miRNAs作为CRPC的新型生物标志物的适用性还有待进一步研究。
原始出处:
C G H Rönnau , S Fussek , F P Smit et al. Upregulation of miR-3195, miR-3687 and miR-4417 is associated with castration-resistant prostate cancer. World J Urol. May 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言




_1583678222000.jpeg)






#miR#
47
#miR-31#
37
#抗性#
33
#去势抵抗性前列腺癌#
33
前列腺癌相关研究,学习了,谢谢梅斯
62