J clin oncol:BRCA1/2致病性变异携带者输卵管卵巢切除术后发生腹膜癌的风险
2022-03-23 Nebula MedSci原创
在输卵管卵巢切除术时患有浆液性输卵管上皮内癌的BRCA1/2致病性变异携带者,随后发生腹膜癌的风险随着时间的推移而升高
上皮细胞性卵巢癌 (EOC) 是最致命的妇科癌症,5年生存率仅47%。一般女性患EOC的终生风险为1.3%,但携带BRCA1或BRCA2致病性变异的女性换EOC的终生平均风险分别是44%和17%。
输卵管卵巢切除术 (RRSO) 是最有效的预防方法,可降低高达96%的EOC风险。为了优化风险降低效果,指南建议BRCA1和BRCA2致病性变异携带者分别在35-40岁和40-45岁时接受RRSO。
但是,虽然RRSO术后卵巢癌风险显著降低,但发展成腹膜癌(PC)的风险仍然存在。腹膜癌的病因至今尚未完全明确,但可能与浆液性输卵管上皮内癌(STIC)有关。本研究旨在评估在进行输卵管卵巢切除术时有无存在浆液性输卵管上皮内癌的女性的腹膜癌风险。
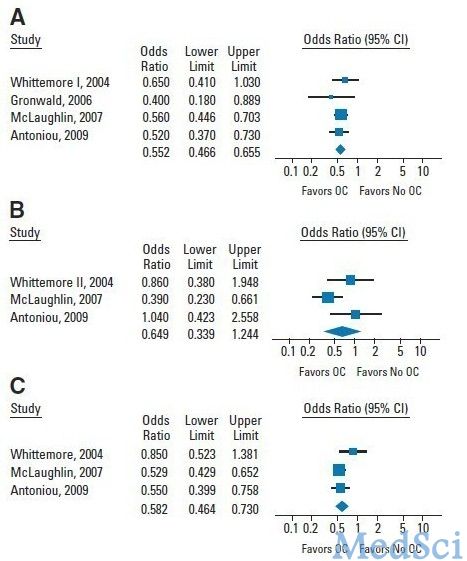
研究人员从EMBASE、MEDLINE和Cochrane数据库中检索了2020年9月之前发表的关于携带BRA1/2致病性变异的接受RRSO的女性的研究。主要指标是在RRSO时有无STIC的BRCA1/2致病性变异携带者发展成腹膜癌的风险比,及术后5年和10年的腹膜癌风险。
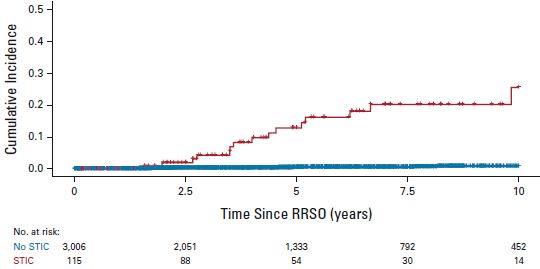
有无STIC的患者发生腹膜癌的累积风险
筛选到了17项符合要求的研究,共涵盖3121位女性,其中115位在输卵管卵巢切除术时存在浆液性输卵管上皮内癌。在随访期间,STIC患者发生PC的风险与无STIC的个体发生PC的风险的比值估计为33.9 (p<0.001)。对于STIC患者,发生PC的5年风险和10年风险分别是10.5%和27.5%,与无STIC个体的相应的风险比分别是0.3%和0.9%。
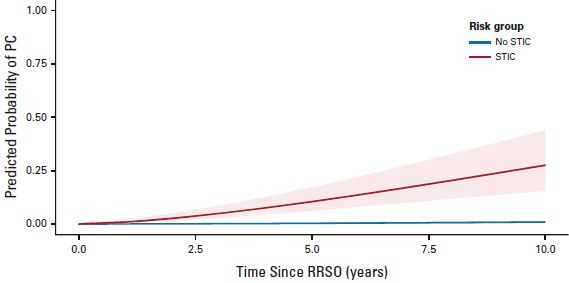
有无STIC的个体发生腹膜癌的预测风险
综上,在输卵管卵巢切除术时患有浆液性输卵管上皮内癌的BRCA1/2致病性变异携带者,随后发生腹膜癌的风险随着时间的推移而升高。
原始出处:
Miranda P. Steenbeek, et al. Risk of Peritoneal Carcinomatosis After Risk-Reducing Salpingo-Oophorectomy: A Systematic Review and Individual Patient Data Meta-Analysis. Journal of Clinical Oncology. March 18, 2022. https://ascopubs.org/doi/full/10.1200/JCO.21.02016.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#致病性#
43
#切除术#
41
#Oncol#
38
#卵巢切除术#
51
#携带者#
46
#输卵管#
0
#腹膜癌#
35
#变异#
32
#BRCA1#
47
#BRCA1/2#
51