柳叶刀风湿病学:系统性硬化症再添新疗法?异基因骨髓衍生的多能间充质基质细胞的安全性和有效性实验
2022-02-10 nobscure MedSci原创
异基因骨髓衍生的多能间充质基质细胞治疗系统性硬化症的安全性和初步疗效:一项单中心、开放标签、剂量递增、概念验证、1/2 期研究。
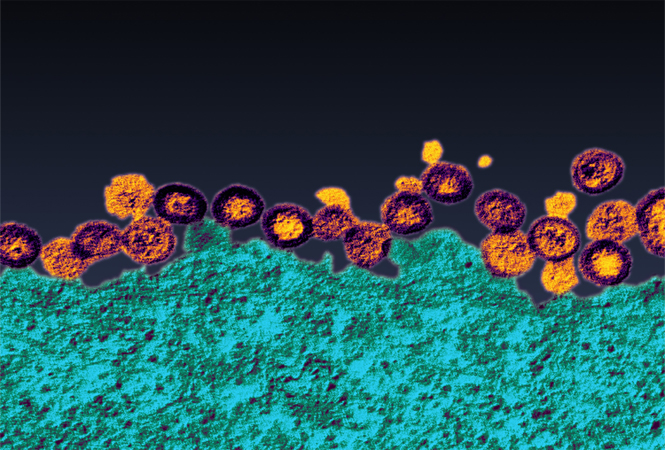
系统性硬化症仍然是一种危及生命的自身免疫性疾病。间充质基质细胞独特的免疫调节、促血管生成和抗纤维化特性为基于间充质基质细胞的系统性硬化症治疗提供了强有力的理论基础,并且间充质基质细胞治疗已在该疾病的临床前模型中显示出益处。尚未确定在严重系统性硬化症患者中使用异基因骨髓来源的间充质基质细胞的安全性。我们旨在测试单次静脉注射家族内同种异体骨髓来源的间充质基质细胞治疗严重弥漫性系统性硬化症的安全性和可行性。
方法
我们在法国巴黎的圣路易斯医院进行了一项开放标签、剂量递增、概念验证的 1/2 期研究。符合条件的患者年龄为 18-70 岁,患有严重的弥漫性系统性硬化症,符合 2013 年美国风湿病学会和欧洲抗风湿病联盟系统性硬化症标准,最低改良 Rodnan 皮肤评分为 15(范围 0-51),患有严重的肺、心脏或肾脏受累,并且对常规免疫抑制疗法或自体造血干细胞移植反应不足或有禁忌症。有严重合并症的患者被排除在外。前十名接受者接受单次静脉输注 1 × 106每公斤体重的骨髓来源间充质基质细胞,随后的十名接受者将被输注单剂量每公斤体重3×10 6 个骨髓来源的间充质基质细胞。主要终点是输注期间和输注后前 10 天内的即时耐受性,以所有输注患者中严重不良事件(3 级或更高级别)的发生来衡量。在 24 个月的随访期间,对所有参与者的安全性进行了评估。
在 2014 年 3 月 24 日至 2020 年 1 月 6 日期间,招募了 20 名患有严重弥漫性系统性硬化症的顺性别个体(13 名女性和 7 名男性)。所有 20 名患者均被纳入主要结果分析。治疗后前10天未发生输液相关严重不良事件,3例输液相关不良事件;一名患者出现 1 级潮红,另一名患者出现 1 级恶心和 2 级乏力。在 10 天和长达 24·1 个月(IQR 20·8-24·5)的中位随访后,14 名 (70%) 患者发生 36 次非治疗相关的严重不良事件,并且没有治疗相关的不良事件被报道。
在患有严重弥漫性系统性硬化症的患者中,单次输注异体骨髓来源的间充质基质细胞是安全的。未来的安慰剂对照试验将有助于明确确定来自各种组织来源的间充质基质细胞治疗对大量系统性硬化症患者的疗效。
来源:Dominique Farge, Séverine Loisel,et.Safety and preliminary efficacy of allogeneic bone marrow-derived multipotent mesenchymal stromal cells for systemic sclerosis: a single-centre, open-label, dose-escalation, proof-of-concept, phase 1/2 study,The Lancet Rheumatology,Volume 4, Issue 2,2022,Pages e91-e104,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#基质#
37
#系统性#
33
#安全性和有效性#
47
#硬化症#
34
#新疗法#
58
#系统性硬化#
38