Nature Medicine: 新晋院士徐兵河论文:治疗耐药性晚期乳腺癌的3期临床试验
2021-11-23 “E药世界”公众号 “E药世界”公众号
乳腺癌是女性最常见的癌症,也在2020年开始成为全世界第一大癌症。激素受体阳性乳腺癌是其主要亚型。内分泌治疗是激素受体阳性乳腺癌治疗的基石,然而,几乎所有患者都出现获得性耐药性。因此,迫切需要新的治疗
乳腺癌是女性最常见的癌症,也在2020年开始成为全世界第一大癌症。激素受体阳性乳腺癌是其主要亚型。内分泌治疗是激素受体阳性乳腺癌治疗的基石,然而,几乎所有患者都出现获得性耐药性。因此,迫切需要新的治疗方法来克服或延缓内分泌抵抗的发生。
细胞周期蛋白依赖性激酶4/6(CDK4/6)通路的过度活跃是激素受体阳性乳腺癌的一个共同特征,通常与内分泌治疗的耐药性有关。达匹西利(Dalpiciclib,SHR6390)是由恒瑞医药开发的新型口服选择性CDK4/6抑制剂。在临床研究中,达匹西利显示出对重度预处理激素受体阳性、HER2阴性乳腺癌患者强大的抗肿瘤活性。
近日,中国医学科学院肿瘤医院徐兵河院士团队团队在国际顶尖医学期刊 Nature Medicine 上发表了题为:Dalpiciclib or placebo plus fulvestrant in hormone receptor-positive and HER2-negative advanced breast cancer: a randomized, phase 3 trial 的研究论文。
该研究报告了一项对中心、随机双盲、安慰剂对照的临床试验的中期结果,这项名为DAWNA-1的3期临床试验,在全国39个中心进行,用于评估达匹西利对比安慰剂加氟维司群治疗既往内分泌治疗复发或进展的激素受体阳性、HER2阴性晚期乳腺癌的效果。
该研究纳入了361名患者,并且达到了主要终点。与安慰剂联合氟维司群治疗的患者相比,接受达匹西利联合氟维司群治疗的患者无进展生存期显着延长,最常见的不良事件为白细胞减少,严重不良事件的发生率与安慰剂组不相上下。因此,该研究结果支持达匹西利联合氟维司群作为激素受体阳性、HER2阴性晚期乳腺癌治疗的新方案。
氟维司群(Fulvestrant)是一类新的雌激素受体拮抗剂,用于治疗激素激素受体阳性晚期乳腺癌。
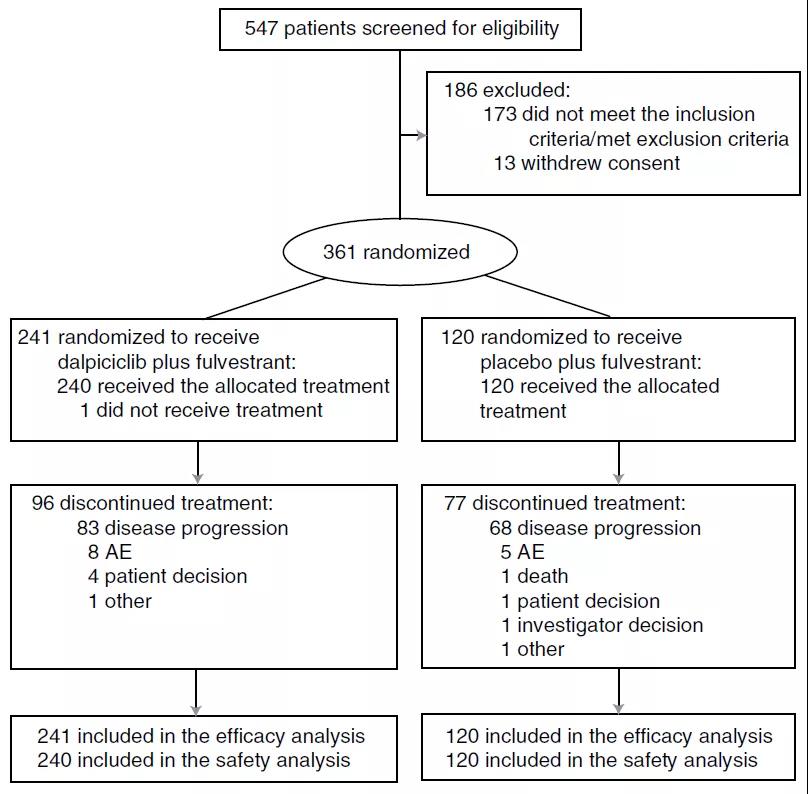
2019年6月25日至2020年9月2日期间,研究团队招募了361名符合条件的患者,这些患者被随机分配到接受达匹西利+氟维司群组(n=241)或安慰剂+氟维司群组(n=120)。两组之间的基线特征基本平衡。总体中位年龄为51.0岁,55.7%的患者为绝经后妇女,60.1%有内脏转移,72.6%曾接受过一种内分泌治疗。
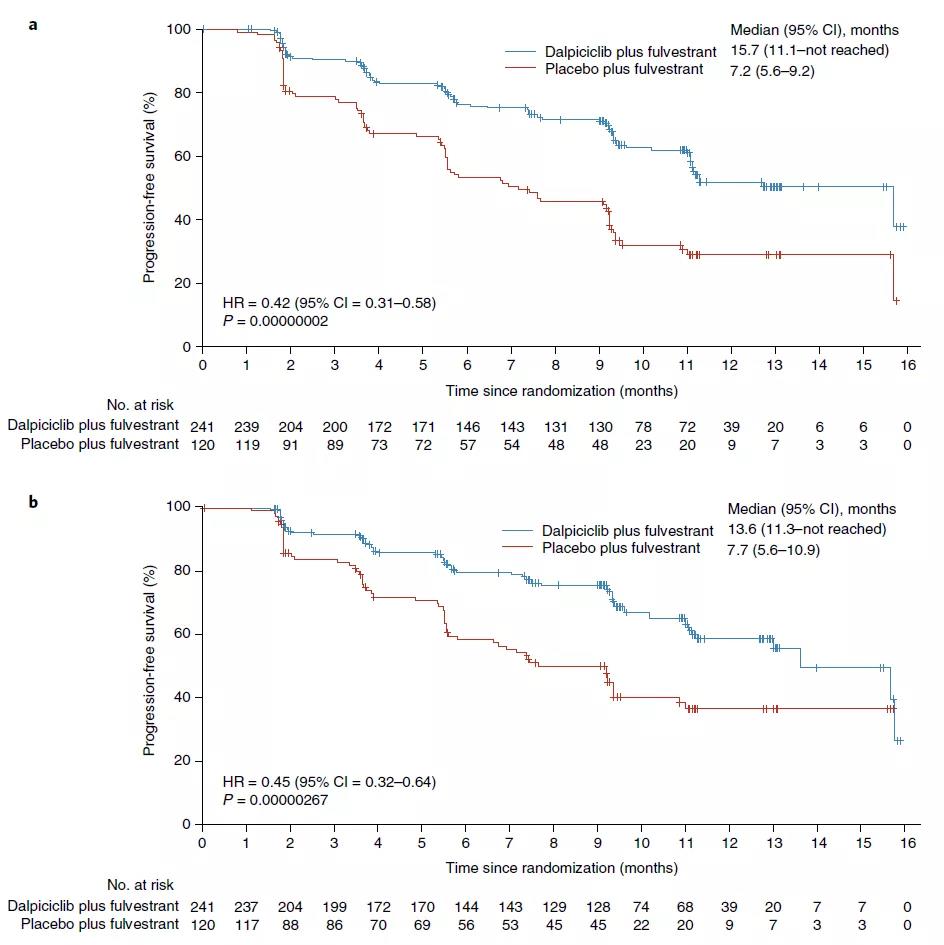
在进行中期分析时,35.7%的治疗组患者和63.3%的安慰剂组患者出现疾病进展或死亡。与安慰剂组相比,治疗组的无进展生存期显着延长:治疗组和安慰剂组在6个月时的无进展生存率分别为76.4%和53.2%,12个月时的无进展生存率分别为51.8%和29.1%。治疗组与安慰剂组的客观有效率分别为27.0%和20.0%,临床受益率分别为61.0%和45.8%。
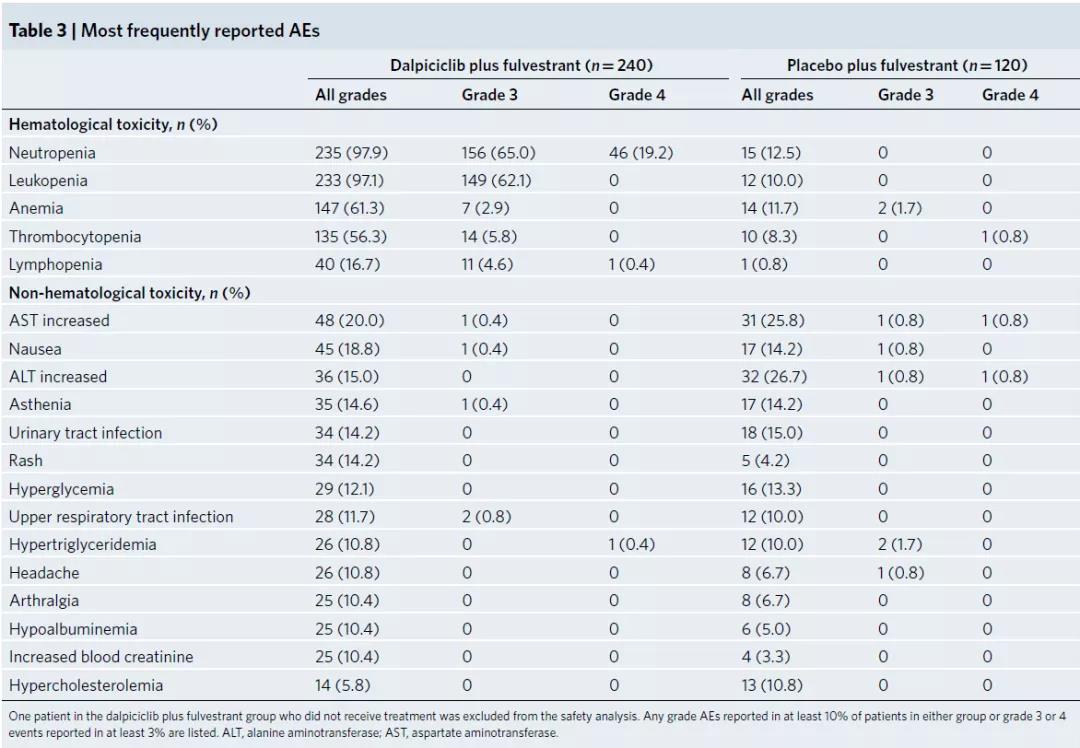
研究团队还评估了达匹西利+氟维司群治疗的安全性。88.3%的治疗组患者和13.3%的安慰剂组患者出现3级或4级不良事件,这些不良事件大部分是源于血液毒性。随着治疗周期的增加,血液毒性的发生率和严重程度呈下降趋势。最常见的非血液学不良事件是低度肝酶异常,两组报告的发病率相当。治疗组中有16例(8.3%)的心电图QT间期延长事件,安慰剂组有1例(0.8%)发生。另外,5.8%的治疗组患者和6.7%的安慰剂组患者出现严重不良事件,其中1例支气管炎,1例肺炎,1例隐球菌性脑膜炎。治疗组有2例(0.8%)患者出现致命性不良事件,安慰剂组有4例出现。
综上,这项3期临床试验表明,达匹西利+氟维司群治疗可显着延长激素受体阳性、HER2阴性晚期乳腺癌的无进展生存期,且安全性可控。这些发现支持将达匹西利联合氟维司群作为一种新的治疗选择,用于治疗对内分泌治疗耐药的激素受体阳性、HER2 阴性的晚期乳腺癌患者。
徐兵河院士
徐兵河,1958年出生,中国医学科学院肿瘤医院/国家癌症中心主任医师、教授,国家新药(抗肿瘤)临床研究中心主任。2021年当选中国工程院院士。
徐兵河专注于乳腺癌领域的前沿理论及技术研究,他带头研发的吡咯替尼是我国首个获批的国产原研创新药物HER-2小分子抑制剂,打破了HER-2靶点被进口药长期垄断的局面,开创了临床试验快速审批上市先河。近5年来,他牵头完成了中国首个获批上市的CDK4/6抑制剂哌柏西利、首个国产CDK4/6药物SHR6390、首个乳腺癌ADC类药物TDM-1、首个中欧双报国产生物类似药HLX02、国内拥有独立自主知识产权的化疗药物优替德隆等一系列抗肿瘤新药的临床试验,为中国抗肿瘤药物的创新研发做出了重大贡献。
原始出处:
Xu, B., Zhang, Q., Zhang, P. et al. Dalpiciclib or placebo plus fulvestrant in hormone receptor-positive and HER2-negative advanced breast cancer: a randomized, phase 3 trial. Nat Med 27, 1904–1909 (2021). https://doi.org/10.1038/s41591-021-01562-9.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CIN#
44
#Nat#
28
#DIC#
44
#3期临床#
39
#徐兵河#
41
#Medicine#
37
#3期临床试验#
39
#Med#
28