Front Oncol:IIIA/N2非小细胞肺癌(NSCLC)患者肺叶切除术对比肺亚叶切除术的疗效
2021-12-11 yd2015 MedSci原创
研究表明, IIIA/N2 NSCLC患者能够从肺亚叶切除或肺叶切除术中获益,且肺叶切除术优于肺亚叶切除术治疗。
很长一段时间对于IIIA/N2非小细胞肺癌(NSCLC)患者来说肺叶切除术的作用存在争议。此外,目前还没有研究关注肺亚叶切除术是否可改善此类患者的预后。因此,来自国内的学者开展了相关研究,比较肺叶切除术和肺亚叶切除术对IIIA/N2非小细胞肺癌(NSCLC)患者的疗效。相关结果发表在Frontiers in Oncology杂志上。
研究是通过筛查2004年至2015年SEER数据库中诊断为IIIA/N2期NSCLC的患者。共有21,638例符合研究标准。研究队列包括未接受手术的患者(n = 15,951),肺亚叶切除术(n = 628)和肺叶切除术(n = 5,059)。使用Kaplan-Meier方法、Cox回归分析和治疗加权逆概率(IPTW)-调整Cox回归来说明研究队列中肺亚叶切除和肺叶切除对总生存率(OS)的影响。
共有21,638例符合研究标准,分为未接受手术的患者(n = 15,951),肺亚叶切除术患者(n = 628)和肺叶切除术患者(n = 5,059)。此外,未手术组13692例,肺叶亚切除术组458例,肺叶切除术组3235例在最后随访前死亡。中位随访时间为81个月,中位生存期为17个月。
肺亚叶切除和肺叶切除治疗患者较未手术患者改善预后,同样,肺叶切除治疗患者较肺亚叶切除患者改善预后。未手术、肺亚叶切除术和肺叶切除术患者的中位生存期分别为14个月、28个月和37个月。3组患者5年OS率(95%CI)分别为11.0%(10.4-11.6%)、25.7%(22.1 -29.8%)和36.4%(34.9-37.9%)。
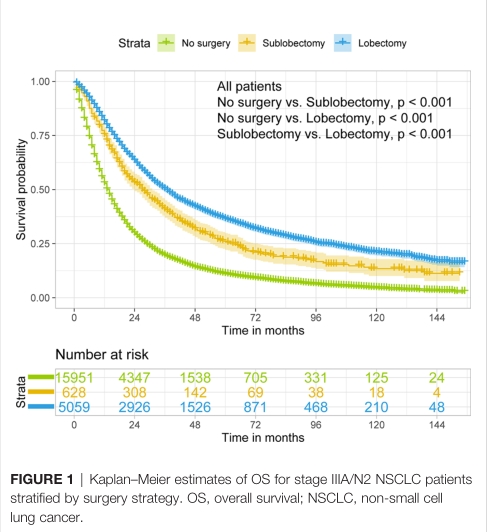
所有患者三组治疗的OS
调整混杂因素的多因素分析,IPTW前,相对于未手术患者,肺亚叶切除和肺叶切除治疗的HR分别为0.584 (95%CI: 0.531–0.644, P-value <0.001) 和0.439 (95%CI: 0.420–0.459, P-value <0.001);IPTW后,HR分别为0.619 (95%CI: 0.605–0.633, P-value <0.001) and 0.441 (95%CI: 0.431–0.451, P-value <0.001)。IPTW前后,相对于肺亚叶切除患者,肺叶切除治疗的HR (95%CI) 分别为0.754 (95% CI: 0.681–0.836, P-value <0.001) 和0.713 (95%CI:0.696–0.731, P-value <0.001)。
基于年龄、肿瘤大小、放疗或化疗的亚组分析中,两手术类型治疗患者的OS均较未手术患者明显改善。年龄<65岁患者,肺叶切除治疗优于肺亚叶切除治疗(P-value <0.001);对于65–72岁和>72岁患者,两手术类型治疗无明显差异(P-value =0.11和P-value = 0.31)。
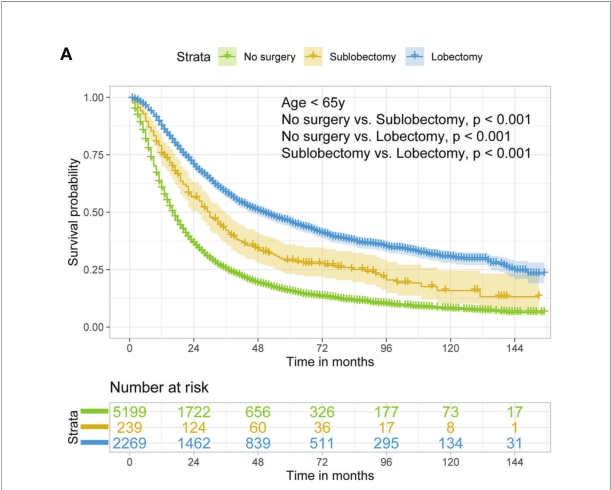


年龄分组三组治疗的OS
基于肿瘤大小来比较两手术类型时发现,肺叶切除治疗均优于肺亚叶切除治疗(all pairwise P-value <0.05)。

肿瘤大小分组三组治疗的OS
在放疗或化疗亚组分析中,肺叶切除在无放疗或化疗的患者中比肺亚叶切除获得更好的OS,在单独化疗或放疗加化疗的患者中也可以看到类似的结果(all pairwise P-value <0.05)。对于接受单独放疗的患者,肺叶下切除术和肺叶切除的结果是相似的,然而,由于样本有限,这一结果说服力不足(P-value = 0.94)。

放化疗分组三组治疗的OS
调整混杂因素的多因素分析,在所有的亚组比较中,肺叶切除治疗均优于肺亚叶切除治疗(HR<1,P-values <0.001)。
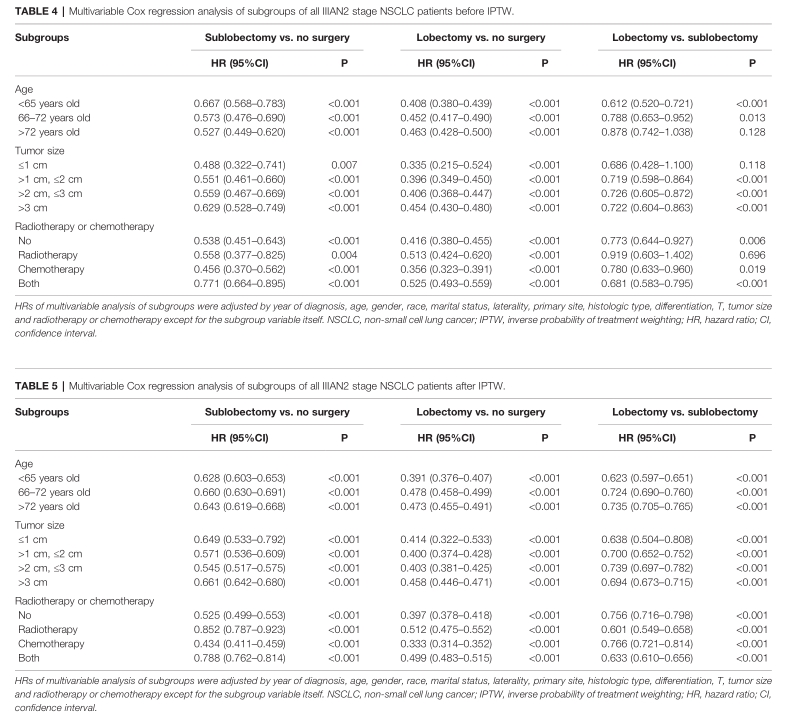
亚组多因素分析
综上,研究表明, IIIA/N2 NSCLC患者能够从肺亚叶切除或肺叶切除术中获益,且肺叶切除术优于肺亚叶切除术治疗。
原始出处:
Wang S, Zhang Z, Gu Y, Lv X, Shi X and Liu M (2021) Lobectomy Versus Sublobectomy in Stage IIIA/N2 Non-Small Cell Lung Cancer: A Population-Based Study. Front. Oncol. 11:726811. doi: 10.3389/fonc.2021.726811
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#III#
35
#非小细胞#
29
#Oncol#
34
#切除术#
31
学习了
70
学习了
47
#肺叶切除#
43
肺叶切除术优于肺亚叶切除术治疗。但是,我建议国内学者对这个研究可以重做一遍,因为不同区域会不一样。随着肺癌治疗的效果越来越好,未来肺叶切除未必优于肺亚叶切除了,相信这个结论会随着时间变化,发生变化。#肺癌#
111
阅国内外无数文献,经过反复推敲和打磨,改版数十次后精心汇编而成
51
学习
48