Mol Psychiatry:抑郁症临床诊断或有生物标记物
2018-11-27 佚名 东南大学
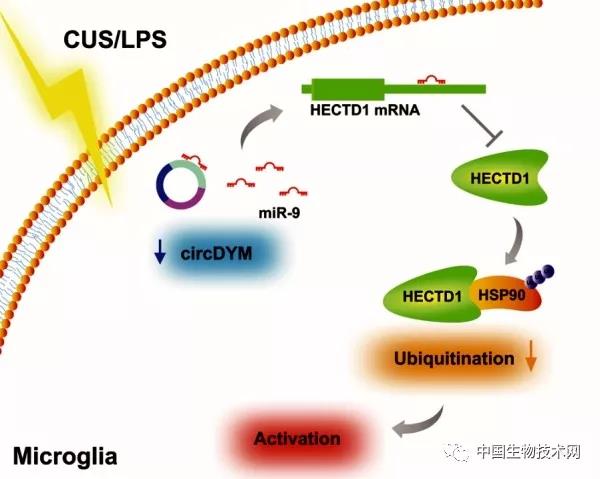
东南大学医学院姚红红教授课题组、东南大学附属中大医院张志珺教授和谢春明研究员课题组以“CircDYM ameliorates depressive-like behavior by targeting miR-9 to regulate microglial activation via HSP90 ubiquitination”为题在Nature出版集团旗下的精神病学杂志《Molecular P
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Psychiatry#
29
#标记物#
36
#生物标记#
24
#生物标记物#
41
#临床诊断#
42