Lancet子刊:神药阿司匹林“再发威”,可降低结直肠息肉复发超6成!
2021-04-03 MedSci原创 MedSci原创
低剂量阿司匹林能安全地抑制FAP患者大于5.0 mm的结直肠息肉的复发。这些结果提示低剂量阿司匹林对FAP有一定的作用,可作为预防FAP结直肠癌的替代方法。
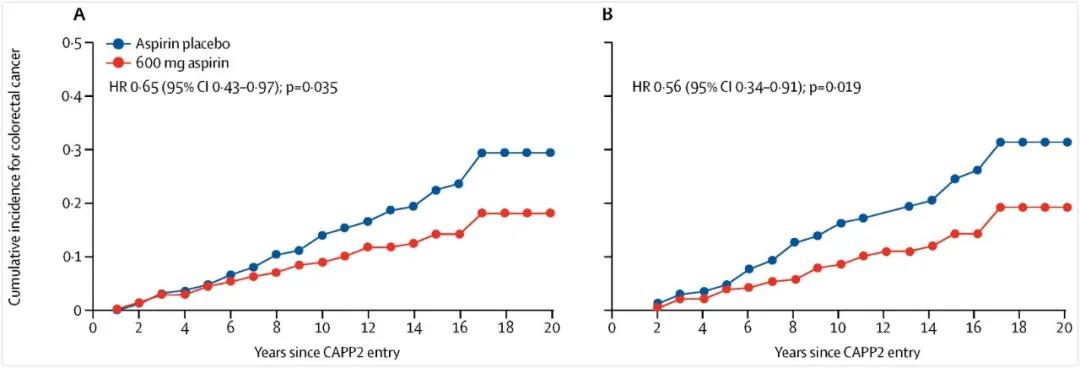
有关阿司匹林预防CRC的证据已有多项顶尖研究证实。尤其是去年6月,发表在《柳叶刀》Lancet杂志上的研究表明,阿司匹林用于预防具有遗传倾向的CRC高危人群,可使此类患者的风险减半,同时效果可长达10-20年!
家族性腺瘤性息肉病(FAP)是一种常染色体显性遗传病,由结肠腺瘤性息肉病基因(APC)突变引起。经典FAP表现为存在100个或更多结直肠腺瘤性息肉,若充分发展可达到数千个结直肠腺瘤,结直肠癌(CRC)风险可高达100%。
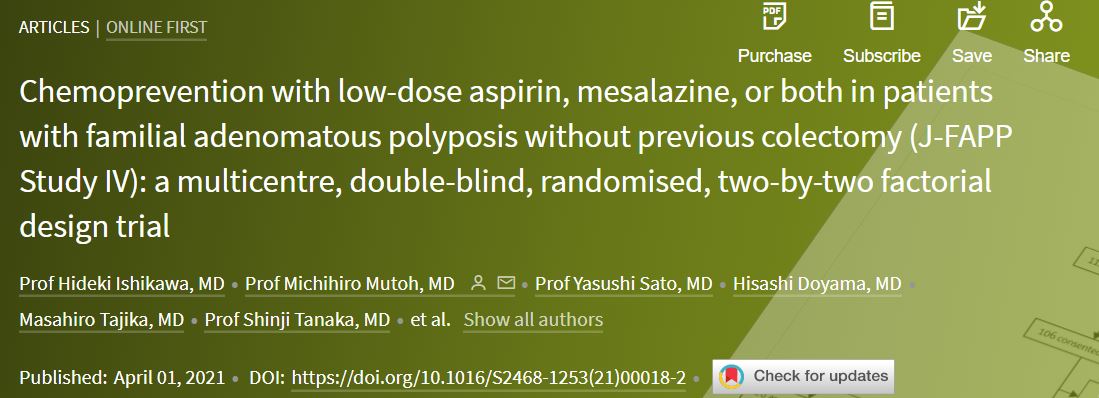
目前,FAP患者预防CRC的唯一既定治疗方法是结肠切除术,这大大降低了患者的生活质量。因此,我们需要一种替代方法。最近,来自日本京都府医科大学的研究人员开展了一项试验,旨在明确低剂量阿司匹林和美沙拉嗪对FAP患者结直肠息肉复发的影响。结果发表在Lancet子刊。
这是一项在日本11个中心进行的随机、双盲、安慰剂对照、多中心试验,采用2对2因子设计。纳入年龄为16-70岁,有大肠腺瘤性息肉病史,无结肠切除术史的参与者。研究前,患者在内镜下切除所有直径至少5.0mm的大肠息肉。
将患者随机分为以下四组:阿司匹林(100mg/d)+美沙拉嗪(2g/d),阿司匹林(100mg/d)+安慰剂,安慰剂+美沙拉嗪(2g/d),或双份安慰剂。8个月后进行结肠镜检查。主要终点是8个月时至少5.0mm的结直肠息肉发生率,在意向治疗人群中评估。
共104名患者被随机分配接受阿司匹林+安慰剂(n=52)或美沙拉嗪+安慰剂(n=52)。总得来说,阿司匹林能降低结肠息肉复发风险63%。在52名未接受阿司匹林的患者中,有26名(50%)在8个月肠镜检查时有至少5.0mm的结直肠息肉,而在50名接受任何阿司匹林的患者中,有15名(30%)患者。
同时,未接受美沙拉嗪的患者中,有21名(42%),在52名接受美沙拉嗪的患者中,这一数字为20名(38%)。接受美沙拉嗪的患者复发的风险为0.87(95% CI 0.38-2.00),差异并不具有统计学差异。
最常见的不良事件是26名接受阿司匹林加美沙拉嗪的患者中有3名(12%)出现1-2级上消化道症状,24名接受阿司匹林加安慰剂的患者中有1名(4%)出现不良事件,26名接受美沙拉嗪加安慰剂的患者中有1名(4%)出现不良事件。
综上,低剂量阿司匹林能安全地抑制FAP患者大于5.0 mm的结直肠息肉的复发。这些结果提示低剂量阿司匹林对FAP有一定的作用,可作为预防FAP结直肠癌的替代方法。
参考文献:
Chemoprevention with low-dose aspirin, mesalazine, or both in patients with familial adenomatous polyposis without previous colectomy (J-FAPP Study IV): a multicentre, double-blind, randomised, two-by-two factorial design trial. https://doi.org/10.1016/S2468-1253(21)00018-2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
27
#结直肠#
34
#结直肠息肉#
39
顶刊就是不一样,质量很高,内容精彩!学到很多
52