Lancet:左主干冠心病患者血管重建-PCI vs CABG,谁更优?
2019-12-24 MedSci MedSci原创
研究发现,PCI在左主干冠心病患者血管重建的5年效果劣于冠状动脉旁路移植术
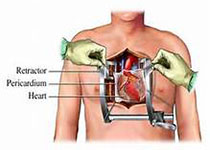
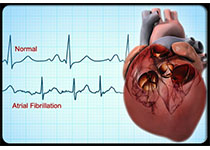
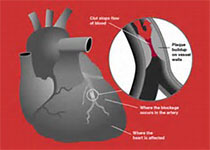
经皮冠状动脉介入治疗(PCI),取代标准的冠状动脉旁路移植术(CABG),被越来越多地应用于左主干冠心病患者的血管重建,NOBLE研究考察了PCI治疗左主干冠状动脉疾病的效果,近日研究人员报告最新的5年随访结果。NOBLE研究中,需血管再通的左主干冠心病患者随机接受PCI或CABG,研究的主要终点为心脏或脑血管重大不良事件(MACCE),包括全因死亡、心肌梗塞、二次血管再通和中风。1201名患者参与研究,其中PCI组598人,CABG组603人。平均随访4.9年,PCI组5年累计MACCE发生率为28%(165例),而CABG组仅为19%(110例),HR=1.58。组间全因死亡率相当(9%,HR=1.08),但PCI组心肌梗塞(8% vs 3%,HR=2.99)以及二次血管再通(17% vs 10%,HR=1.73)风险增加。研究发现,PCI在左主干冠心病患者血管重建的5年效果劣于冠状动脉旁路移植术。原始出处:Niels R Holm et al. Percutaneous coronary angioplasty versus coronary artery bypass graf
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了
70
#Lancet#
41
#左主干#
35
#冠心病患者#
30